Blood:北美ATLL患者具有独特的突变和表观遗传图谱,有望采用表观遗传治疗
2018-08-15 qinqiyun MedSci原创
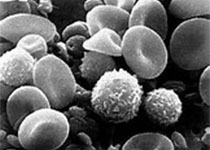
中心点:北美ATLL患者具有独特的遗传图谱,携带高频的与预后相关的表观遗传突变,包括EP300突变。携带EP300的ATLL样本,p53功能受损,对地西他滨治疗敏感性多变。摘要:成人T细胞白血病淋巴瘤(ATLL)是一种罕见的T细胞肿瘤,好发于日本、加勒比海和拉丁美洲人群。大部分北美ATLL患者为加勒比人后裔,与日本ATLL患者相比,其特征为化疗耐受性疾病发病率高、预后差。为明确两个队列的遗传差异,
中心点:
北美ATLL患者具有独特的遗传图谱,携带高频的与预后相关的表观遗传突变,包括EP300突变。
携带EP300的ATLL样本,p53功能受损,对地西他滨治疗敏感性多变。
摘要:
为明确两个队列的遗传差异,研究人员对30位北美ATLL患者进行靶向外显子测序,并将结果与日本ATLL病例进行对比。虽然两个队列的TP53突变频率相当,但表观遗传和组蛋白修饰基因的突变频率(57%)明显高于日本队列,而JAK/STAT和TCR/NF-κB信号通路基因的突变频率又显著低于日本队列。
最常见的表观遗传突变是会影响EP300(20%)的基因。在一定范畴内,表观遗传突变与预后不良相关。此外,研究人员通过对9例原发患者病例进行RNA-seq分析也发现了北美ATLL患者与日本ATLL患者之间存在差异。携带突变型EP300基因的ATLL患者样本,p53蛋白总量和乙酰化p53蛋白均减少,并具有与p53突变型癌症相似的转录特征。
更为重要的是,在EP300突变型ATLL样本中,地西他滨具有高度的选择性单药活性,提示地西他滨治疗可诱导EP300突变型ATLL细胞合成性致死。
总而言之,本研究表明北美ATLL患者具有独特的遗传图谱,特征是表观遗传突变频繁,或可采用DNMT抑制剂进行预临床靶向治疗。
原始出处:
Urvi A. Shah,et al. North American ATLL has a distinct mutational and transcriptional profile and responds to epigenetic therapies. Blood 2018 :blood-2018-01-824607; doi: https://doi.org/10.1182/blood-2018-01-824607
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ATLL#
22
#ATL#
33
不错的文章值得拥有哦
51
了解一下,谢谢分享!
57
学习了
52