JEADV:分泌型白细胞蛋白酶抑制剂调节银屑病中神经反射介导的皮肤屏障功能
2022-03-19 医路坦克 MedSci原创
分泌性白细胞蛋白酶抑制因子(SLPI)是天然免疫和获得性免疫的重要调节因子,本文通过SLPI缺陷小鼠和咪喹莫特诱导的银屑病实验模型评估SLPI在银屑病中的作用。
银屑病是一种慢性炎症性皮肤病。尽管目前有多种治疗方法用于消除银屑病的症状,但尚无治愈方法。最有效的调节疗法是基于用生物制剂中和特定的炎症介质,如IL-17和IL-23。这种方法主要针对失调的免疫反应。因此,有必要关注在疾病进展早期可能被激活的较少描述的分子和细胞皮肤成分,包括抗菌肽(AMPs)和周围神经。β的过度表达是银屑病皮肤的标志之一。这些AMP被认为在皮肤炎症中起调节作用,一般情况下加重银屑病皮肤损害,但也有助于恢复内环境稳定。例如,LL-37和/或β防御素可以通过在树突状细胞和/或角质形成细胞中启动自身DNA或自身RNA介导的反应来推动皮肤炎症。另一方面,也发现LL-37还阻止了对DNA敏感的炎性小体的激活,这表明它在银屑病中具有抗炎作用
在银屑病患者皮肤中高度表达的AMPs是分泌性白细胞蛋白酶抑制物(SLPI)。尽管SLPI参与了控制微生物的生长,但该蛋白最著名的作用是它对丝氨酸蛋白酶的抑制作用,如中性粒细胞弹性蛋白酶。SLPI在皮肤病理生理学中的作用尚不清楚。在皮肤损伤模型中,SLPI被证明能促进损伤皮肤的修复。SLPI还可以通过修饰DNA和促进血浆细胞样树突状细胞中TLR9的激活,以及通过抑制中性粒细胞外陷阱(NETS)的沉积来在皮肤中发挥免疫调节作用。这些作用表明SLPI在银屑病的病理生理中对这种分子起着重要的调节作用。
在这里,我们显示SLPI缺乏导致的病理性皮肤变化超出咪喹莫特(ImQ)诱导的银屑病实验模型中的皮肤变化,并且这些扩展的皮肤变化是神经反射弧介导的调节失调的通路的结果。我们的数据表明,与神经系统对话的SLPI参与控制银屑病的时空定义参数,并可能改善银屑病病理所固有的表皮内稳态的破坏。
对银屑病发展的早期阶段缺乏了解是成功干预皮肤病理的主要障碍。我们推测SLPI和可能在疾病发展早期被激活的外周神经可能形成一种功能关系,以维持皮肤屏障的动态平衡,并对各种威胁做出反应。
我们使用健康供者和银屑病患者的皮肤活检组织来显示SLPI的表达模式。在SLPI缺陷小鼠和咪喹莫特诱导的银屑病实验模型中,对SLPI在银屑病中的作用进行了机械评估。
我们发现缺乏SLPI的小鼠在咪喹莫特诱导的银屑病中有超出治疗部位的夸大的皮肤变化。与野生型小鼠相比,SLPI缺陷小鼠的皮肤反应在时空上截然不同,这是由于皮肤屏障功能受损,表现为通过咪喹莫特挑战皮肤周围更大的皮肤区域,增加了经皮水分损失。在缺乏SLPI的情况下,增加的致病性皮肤变化可以通过阻断神经反射弧的药物治疗而逆转。
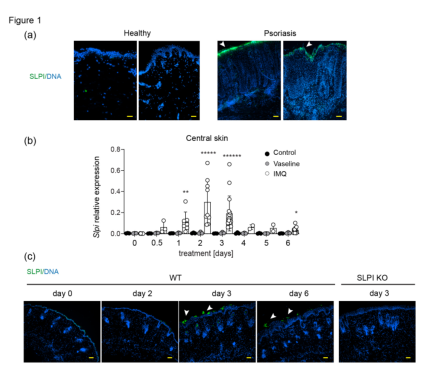
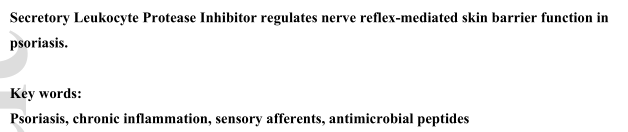
图1 SLPI在牛皮癣患者皮损和牛皮癣实验模型中的表达增加。(A)来自捐赠者的人体皮肤的荧光显微镜图像。图中显示了来自2名健康人和2名银屑病患者的重叠图像。每组至少有4名捐助者的数据具有代表性。(B)C57BL/6小鼠在ImQ和凡士林治疗过程中SLPI基因表达的变化。对照组=未处理的小鼠。数据以3个独立实验的平均值±SD表示。圆点表示单个老鼠。*,p<0.00001;**,p<0.00001;*,p<0.000001;经KruskalWallis多重比较检验。(C)ImQ治疗过程中小鼠皮肤中SLPI蛋白表达的代表性图像。皮肤切片进行SLPI(绿色)和DNA(蓝色)染色。数据来自一个实验,代表了至少五个实验。来自SLPI KO小鼠的图像显示为阴性对照。空调中的箭头指向SLPI染色的表皮。比例尺=50μm。

图2 SLPI影响IMQ挑战部位以外的皮肤损伤的大小和皮肤屏障功能。指定的小鼠接受ImQ治疗,随后对病变大小和皮肤红斑进行动态评估。(A)显示了来自C57BL/6×129/SVJ混合背景的雌性WT和SLpi KO小鼠的代表性图像和指定的治疗部位。(B)显示病变大小的累积数据(平均值±扫描电子显微镜)。N=3~10只/组。(C)显示皮肤红斑的累积数据(平均值±扫描电子显微镜)。(D)WT和SLPI KO C57BL6男性在中央和侧面皮肤指示的日期接受ImQ治疗,然后进行TEWL测量。给出了平均值±扫描电子显微镜。N=每组至少10只小鼠。(E)给WT和SLPI KO C57BL6雄性小鼠注射0.9%的氯化钠。在IMQ治疗前的刺激部位。然后在中央和侧面皮肤指示的日期测量TEWL。给出了平均值±扫描电子显微镜。N=每组至少7只小鼠。(F)在指定的天数取WT小鼠外侧皮肤,进行SLPI mRNA水平的定量聚合酶链式反应分析。数据以3个独立实验的平均值±SD表示。圆点表示单个老鼠。**,p<0.001;**,p<0.01;*,p<0.05;

图3.SLPI缺乏不影响牛皮癣的皮肤厚度,对实验性牛皮癣的皮肤炎症只有轻微影响。WT和SLpi KO C57BL/6雄性小鼠接受IMQ治疗。(A)皮褶厚度是用卡尺在标明的日期测量的。给出了平均值±扫描电子显微镜。N=3~10只/组。*p<0.00001.0 1;**,p<0.0 1;(B)取皮肤进行组织学分析。这些结果代表了至少三个独立的实验。(C)取皮肤进行流式细胞仪分析。用抗CD45单抗检测白细胞总数,用抗Ly6G和CD11b单抗检测中性粒细胞,用抗CD3单抗检测T细胞。N=7-10只小鼠的平均值为±SD。经t检验,P<0.05。
图4 SLPI以神经反射弧控制的方式防止皮肤区域的水分流失。向WT或SLPI KO C57BL/6小鼠腹膜内施用5mM BUV或载体(0.9%NaCl),然后进行IMQ处理。(a) 在指定的天数测量TEWL并以平均值±SEM表示。n=每组7-9只小鼠。*,p<0.05;******,p<0.00001;由ANCOVA进行,然后进行Bonferroni事后测试。(b) 在指定的天数使用手动评分评估皮肤损伤的面积,并以平均值±SEM表示。每组n=7-9只小鼠。(c) 在qPCR指示的天数分析用0.9%NaCl(空心条)或BUV(阴影条)处理的WT小鼠中的Slpi mRNA水平。数据显示为平均值±SD,并且在第3天和第6天相对于NaCl处理的中央和后期皮肤呈现。n=3次实验,数据点显示个体小鼠*Mann-Whitney U检验p<0.05。
总之,这些数据表明SLPI通过防止银屑病发病机制中固有的皮肤干燥而在银屑病中起到保护作用,而且这种SLPI作用依赖于以反射方式操作的神经元输入。这些发现揭示了一种以前未知的维持皮肤动态平衡的机制,这种机制涉及神经系统和一种蛋白质之间的串扰,从解剖学上讲,蛋白质可以加强表皮通透性屏障。
文献来源:Kwiecinska P, Grygier B, Morytko A, Secretory Leukocyte Protease Inhibitor regulates nerve reflex-mediated skin barrier function in psoriasis.J Eur Acad Dermatol Venereol 2022 Mar 12;

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EADV#
53
#分泌#
41
#抑制剂#
37
#屏障功能#
47
#皮肤屏障#
53
#蛋白酶#
50
学习了
48
好文章,谢谢分享。
67