NEJM:Tepotinib治疗MET外显子14跳跃突变非小细胞肺癌II期临床效果显著
2020-09-03 MedSci原创 MedSci原创
对于MET外显子14跳跃突变的晚期非小细胞肺癌患者,Tepotinib治疗应答率在50%左右,最常见的3级以上不良事件为外周水肿
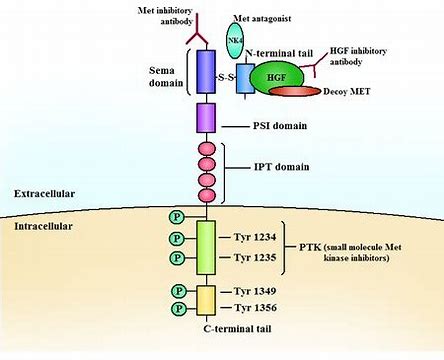
在非小细胞肺癌(NSCLC)患者中,3-4%的患者由于剪接位点突变,导致致癌驱动基因MET第14外显子出现转录缺失。研究人员评估了一种高选择性MET抑制剂Tepotinib对MET14外显子跳跃突变患者的疗效和安全性。
本次研究为II期临床研究,招募MET14外显子跳跃突变的晚期或转移性NSCLC患者,患者接受500mg的Tepotinib治疗,每天一次,随访至少9个月。研究的主要终点是客观反应,对患者体液及组织样本中MET14外显子跳跃突变情况进行分析。
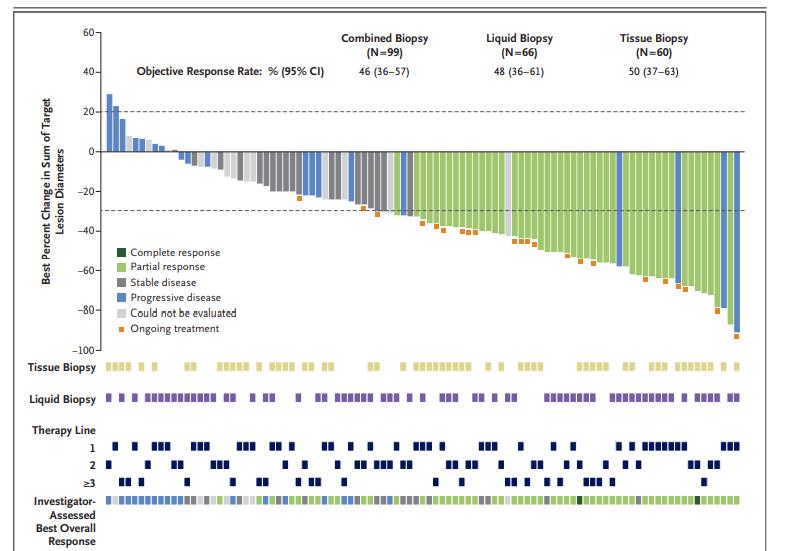
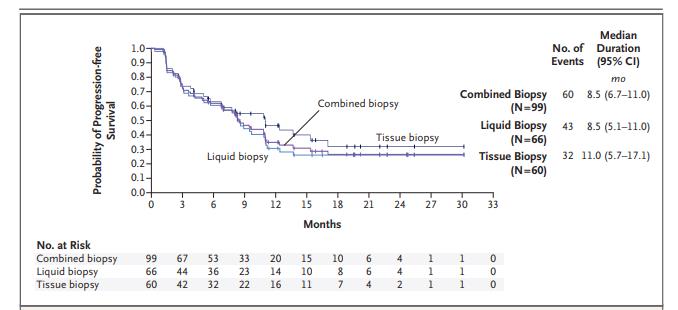
截至2020年1月1日,共有152名患者接受了Tepotinib治疗,99名患者接受了至少9个月的随访。独立审查显示Tepotinib治疗应答率为46%,中位持续时间为11.1个月。体液活检组66例患者的应答率为48%,组织活检组60例患者的应答率为50%。研究者评估的治疗应答率为56%。
28%的患者报告了与Tepotinib治疗有关的3级或更高级不良事件,外周水肿发生率为7%。11%的患者因不良事件停药。通过循环游离DNA检测,67%的患者观察到分子水平的治疗响应。
研究认为,对于MET外显子14跳跃突变的晚期非小细胞肺癌患者,Tepotinib治疗应答率在50%左右,最常见的3级以上不良事件为外周水肿。
原始出处:
Paul K. Paik et al. Tepotinib in Non-Small-Cell Lung Cancer with MET Exon 14 Skipping Mutations. N Engl J Med, September 3 , 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#I期临床#
21
#MET#
32
#非小细胞#
22
#tepotinib#
36
#临床效果#
32
#II期临床#
26
#外显子#
31
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
51
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
48