Sci Rep:开始诊断的黑色素瘤能够增加随后患前列腺癌风险
2018-05-21 AlexYang MedSci原创
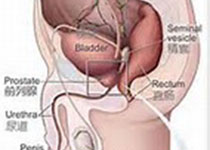
越来越多的证据表明,皮肤黑色素瘤的诊断(CM)也许与前列腺癌的发生率(PC)相关。最近,有研究人员调查了是否CM的发生率与随后PC风险的增加相关。研究人员利用来自新南威尔士癌症数据库中的所有CM和PC案例数据进行了分析,这些案例都在1972年和2008年之间诊断。研究人员针对PC发生率计算了年龄标准化发生率(SIR)和95%置信区间(95% CI)。另外,研究人员还根据指定的社会人口统计学分类和疾
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺癌风险#
33
#色素#
0
#癌风险#
32
#黑色素#
33
#黑色素#
0
学习了谢谢
51
^_^^_^^_^
59
学习
57