背景介绍:
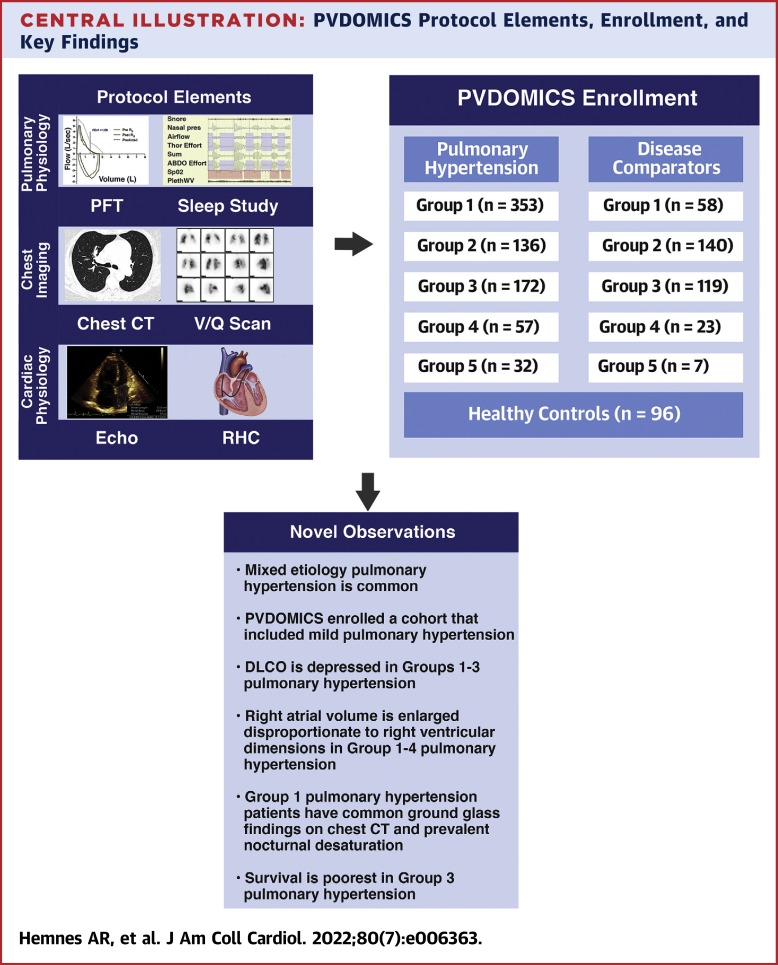
PVDOMICS(肺血管疾病表型学)是一项精准医疗计划,利用深度表型来描述肺血管疾病(PVD)。PVDOMICS测试的假设是,将临床指标与全局指标结合起来,将加强对PVD的理解,并促进更新PVD分类。
研究目的:
本研究的目的是描述PVDOMICS队列的临床特征和无移植生存率。
研究方法:
世界肺动脉高压研讨会(WSPH)第1-5组的PH患者、具有类似基础疾病和轻度或无PH的疾病比较者以及健康对照者参加了一项横断面研究。PH组、比较者使用标准的统计学测试进行比较,包括比较移植或死亡时间的对数rank测试。这个临床研究网络包括美国各地的7个中心(布莱根妇女医院、哈佛医学院、哥伦比亚大学欧文医学中心、威尔康奈尔医学中心、约翰霍普金斯医院、梅奥诊所[罗切斯特]、亚利桑那大学[图森]和范德比尔特大学医学中心)和克利夫兰诊所的一个数据协调中心。参与者被纳入一项前瞻性的纵向队列研究(NCT02980887)。PVDOMICS招募了1226名受试者,最终分析中包括1193人,包括96名健康对照受试者,347名比较者和750名PH患者(图1)。按WSPH组别划分,有353名第1组、136名第2组、172名第3组、57名第4组和32名第5组的入组者。比较者包括58名第一组,140名第二组,119名第三组,23名第四组和7名第五组受试者。
研究结果:
总共有1,193名受试者被纳入。在38.9%的PH受试者中发现了多个WSPH组。在第1、第3和第4组PH与比较者相比,更经常观察到夜间饱和度降低。第1组PH受试者中共有50.2%的人在胸部计算机断层扫描中出现了磨玻璃不透明。1-3组PH的一氧化碳扩散能力明显低于其各自的对比者。WSPH第1-4组的右心房容积指数高于对比者。共有110名参与者的平均肺动脉压力为21-24mmHg。第3组PH值的无移植生存率最差。
研究结论:
PVDOMICS招募了整个PVD谱系的受试者,包括轻度和混合病因的PH。新发现包括一氧化碳扩散能力低和右心房容积指数增大分别是1-3组和1-4组PH的共同特征;计算机断层扫描中意外地经常出现磨玻璃样斑点;1组PH有睡眠改变,3组PH的生存率最差。PVDOMICS将促进对PVD的新认识,并完善目前的PVD分类。(肺血管疾病表型组学项目PVDOMICS[PVDOMICS];NCT02980887)
参考文献:
Hemnes AR, Leopold JA, Radeva MK, Beck GJ, Abidov A, Aldred MA, Barnard J, Rosenzweig EB, Borlaug BA, Chung WK, Comhair SAA, Desai AA, Dubrock HM, Erzurum SC, Finet JE, Frantz RP, Garcia JGN, Geraci MW, Gray MP, Grunig G, Hassoun PM, Highland KB, Hill NS, Hu B, Kwon DH, Jacob MS, Jellis CL, Larive AB, Lempel JK, Maron BA, Mathai SC, McCarthy K, Mehra R, Nawabit R, Newman JH, Olman MA, Park MM, Ramos JA, Renapurkar RD, Rischard FP, Sherer SG, Tang WHW, Thomas JD, Vanderpool RR, Waxman AB, Wilcox JD, Yuan JX, Horn EM; PVDOMICS Study Group. Clinical Characteristics and Transplant-Free Survival Across the Spectrum of Pulmonary Vascular Disease. J Am Coll Cardiol. 2022 Aug 16;80(7):697-718. doi: 10.1016/j.jacc.2022.05.038. PMID: 35953136.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺血管疾病#
29
#临床特征#
40
dg
0
#JACC#
35
#生存率#
50
#ACC#
31
#血管疾病#
25