Arthritis Rheumatol:DETECT算法可准确预测系统性硬化症患者的肺动脉高压风险
2021-03-25 Nebula MedSci原创
肺动脉高压(PAH)是导致系统性硬化症患者死亡的主要原因之一
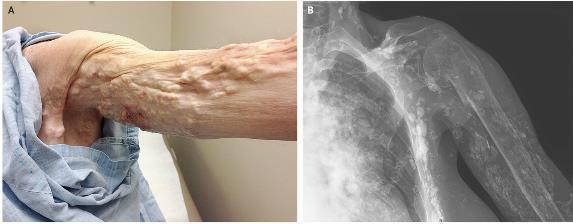
系统性硬化(SSc)是一种累及多器官系统的自身免疫性疾病,以纤维化、炎症和血管损伤为特征。肺动脉高压(PAH)是导致SSc患者死亡的主要原因之一。
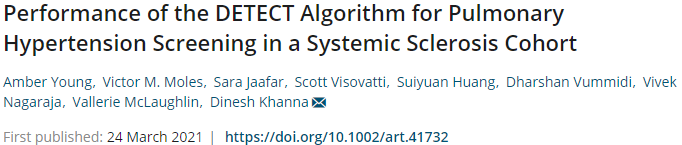
本研究在接受右心导管(RHC)进行肺高压(PH)评估的SSc队列中,评估了DETECT算法和2015年欧洲心脏病学会/欧洲呼吸学会(ESC/ERS)指南的预测准确性。
纳入经RHC明确无PH或有PAH的SSc患者,且要求有DETECT和2015 ESC/ERS指南的应用变量数据。根据2018年修订后的高分辨率CT肺纤维化标准和程度基于血流动力学进行PH分类。分别测试了DETECT算法和2015 ESC/ERS指南的灵敏度和预测准确性,包括DLCO≥60%的受试者的分析。
DETECT和2015 ESC/ERS指南的预测准确性
68例SSc患者接受了RHC检查,其中58例无PH,10例有PAH。队列的平均年龄为60.0岁,58.8%的患者存在局限性皮肤SSc。DETECT算法的灵敏度为1.00(95%CI 0.69~1.00),阴性预测值(NPV)为1.00(0.80~1.00),而2015 ESC/ERS指南的灵敏度为0.80(0.44~0.97),NPV为0.94(0.81~0.99)。
在DLCO≥60%(N=27)的受试者中,DETECT算法的敏感度为1.0(0.29-1.00),NPV为1.00(0.59-1.00),而2015 ESC/ERS指南的敏感度为0.67(0.09-0.99),NPV为0.94(0.71-1.00)。
总之,DETECT算法对包括DLCO≥60%的诊断PAH具有较高的灵敏度和阴性预测值。
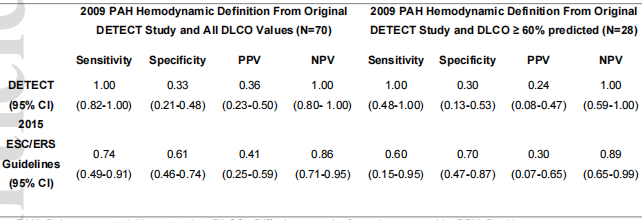
原始出处:
Young Amber,Moles Victor M,Jaafar Sara et al. Performance of the DETECT Algorithm for Pulmonary Hypertension Screening in a Systemic Sclerosis Cohort. Arthritis Rheumatol, 2021, https://doi.org/10.1002/art.41732
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TEC#
35
#系统性#
25
#动脉高压#
24
#硬化症#
30
#Arthritis#
33
#ART#
28
#系统性硬化#
25
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
53