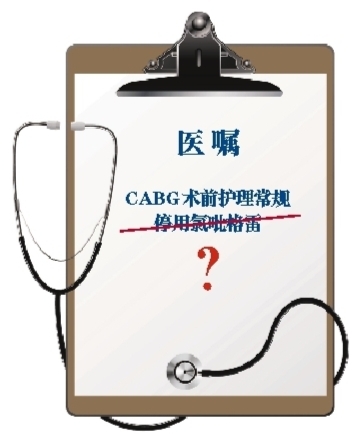
氯吡格雷能否“走进”手术室?
2011-06-10 郑哲 MedSci原创
一项荟萃分析对34项研究中22854例因急性冠状动脉综合征(ACS)接受冠状动脉旁路移植术(CABG)治疗的患者进行研究后发现,术前停用氯吡格雷与否,对死亡、CABG术后心肌梗死、卒中和联合主要不良心血管事件发生率无影响。研究5月24日在线发表于《欧洲心脏杂志》(Eur Heart J)。 在CABG术前,氯吡格雷要不要停药,这是一个问题。为此,我们采访了该荟萃分
一项荟萃分析对34项研究中22854例因急性冠状动脉综合征(ACS)接受冠状动脉旁路移植术(CABG)治疗的患者进行研究后发现,术前停用氯吡格雷与否,对死亡、CABG术后心肌梗死、卒中和联合主要不良心血管事件发生率无影响。研究5月24日在线发表于《欧洲心脏杂志》(Eur Heart J)。 在CABG术前,氯吡格雷要不要停药,这是一个问题。为此,我们采访了该荟萃分析第一作者、英国伦敦帝国学院卫生保健国民卫生服务体系信托机构苏欣德·尼耶(Sukhjinder S. Nijjer)教授,以及中国医学科学院阜外心血管病医院郑哲教授。 在等待中度过的患者 提到冠心病介入治疗后减少血栓事件,氯吡格雷的有效抗血小板作用不容忽视。 在很多心脏中心,ACS患者在接受冠状动脉造影和经皮冠状动脉介入(PCI)术治疗之前,常被给予氯吡格雷,以确保血小板功能在支架置入术中的有效抑制,但还有10%~15%的患者需要通过CABG实现血运重建。目前这些患者在CABG术前只能在等待中度过,等待他们被抑制的血小板功能恢复。 让心外科医生“头疼”的氯吡格雷 氯吡格雷在CABG
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








郑教授,赞一个
144
受教了
94
#手术室#
41
Wow! Great tnhiking! JK
112