PNAS:新研究有助于治疗骨质疏松
2020-08-10 EMILY LEE 细胞
骨质疏松症是最常见的与年龄相关的骨骼疾病,它影响着全球数亿人群。据估计,年龄在50岁以上的女性中,三分之一的女性和五分之一的男性患有骨质疏松性骨折。
骨质疏松症是最常见的与年龄相关的骨骼疾病,它影响着全球数亿人群。据估计,年龄在50岁以上的女性中,三分之一的女性和五分之一的男性患有骨质疏松性骨折。
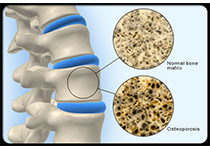
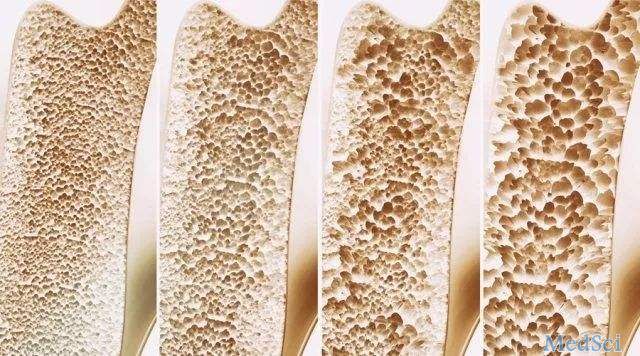
骨质疏松症是由骨吸收细胞的过度活化,而骨形成细胞的活性降低引发的症状。在健康个体中,这两种细胞活性的平衡可以使骨骼不断更新,从而保持骨骼健康和强壮。
在骨质疏松症中,骨吸收不成比例会导致骨矿物质密度低,从而导致骨骼脆弱且容易骨折。当新的骨形成无法赶上骨质流失时,骨最终会变弱,并且更容易发生骨折。
当前大多数骨质疏松症治疗方法包括使用双膦酸盐,其可阻断骨吸收细胞的活性,从而防止骨吸收过多。但是,长期使用这些药物有可能导致骨折风险增加和其他不良副作用。因此,迫切需要开发克服当前治疗方法局限性的新策略。
最近,来自新加坡国立大学新加坡国立大学生物科学系Christoph Winkler教授和德国JMU的Manfred Schartl教授合作开发了一项新技术有助于骨质疏松症的治疗,相关结果发表在PNAS杂志上。
研究小组使用小型鱼模型(Oryzias latipes)进行遗传分析,鉴定出了一种蛋白,即趋化因子CXCL9,在骨质疏松条件下,该蛋白向容纳骨吸收细胞前体的“库”中扩散。这些前体在其细胞表面产生受体CXCR3。通过CXCL9激活后,这些前体被动员并以高度定向的方式向骨基质迁移,并在此开始吸收骨质。
众所周知,CXCL9及其受体CXCR3都能调节免疫细胞向炎症部位的迁移,例如在牛皮癣和类风湿性关节炎发生过程中。尽管阻断CXCR3活性的化学抑制剂在治疗牛皮癣的临床试验中几乎没有成功,研究小组表明,这些抑制剂在阻止骨吸收细胞的募集和保护骨免受骨质疏松性损伤方面非常有效。
Schartl和Winkler教授的结论是:“我们的研究为骨质疏松症治疗提供了新途径。该方法允许对募集到骨基质中的破骨细胞数量进行微调,而不是像传统疗法那样广泛阻止破骨细胞活性。这可以有针对性地防止过度的骨吸收,但是正常的骨转换仍将继续,这有可能避免骨质疏松症患者骨折风险的增加,并保持健康的骨骼以改善生活质量。”
原始出处:
Quang Tien Phan, Wen Hui Tan, Ranran Liu, et al.Cxcl9l and Cxcr3.2 regulate recruitment of osteoclast progenitors to bone matrix in a medaka osteoporosis model.Proc Natl Acad Sci U S A. 2020 Jul 27;202006093. doi: 10.1073/pnas.2006093117.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











mark
60
#PNAS#
0
学习了
91
#骨质#
37
很好
99