JAHA:HIV患者血清PCSK9水平与冠脉内皮功能呈负相关
2018-09-30 MedSci MedSci原创
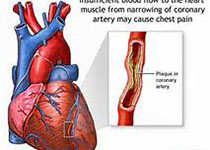
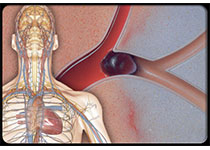
HIV阳性病人患冠心病的风险会增高,但具体机制尚未阐明。本研究纳入分析了48例接受抗病毒治疗的无冠心病的HIV阳性患者,以及15例年龄和低密度脂蛋白胆固醇匹配的正常对照,对其进行磁共振检查以评估冠脉内皮功能,并抽取血样检测血清PCSK9水平和血管标志物水平。分析结果显示,HIV阳性患者的血清PCSK9水平高出正常对照65%(P<0.0001),且HIV患者的冠脉内皮功能明显降低,并与血清PC
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HIV患者#
35
#Csk#
39
#PCS#
38
#AHA#
36
#内皮功能#
44
#负相关#
33