Eur J Cancer:曲妥珠单抗-拉帕替尼新辅助治疗HER2+早期乳腺癌患者的疗效:来自CHER-Lob研究
2021-07-19 yd2015 MedSci原创
Cher-LOB研究生存分析证实pCR和TILs的预后作用,同时提示曲妥珠单抗联合拉帕替尼较曲妥珠单抗可改善患者预后倾向。
II期随机临床研究Cher-LOB主要是评估曲妥珠单抗-拉帕替尼在HER2+早期乳腺癌中新辅助治疗的疗效。主要纳入II-IIIA 期HER2阳性乳腺癌患者,随机(1:1:1)分为接受紫杉醇-蒽环类化疗联合曲妥珠单抗(A组)或拉帕替尼(B组)或曲妥珠单抗+拉帕替尼(C组)作为新辅助治疗。前期分析结果表示,曲妥珠单抗+拉帕替尼联合化疗新辅助治疗较曲妥珠单抗或拉帕替尼联合化疗明显提高病理完全缓解(pCR)率。近期,European Journal of Cancer杂志更新了该研究的结果。
A、B和C三组分别有36, 39 和46例患者。中位随访9年(95% CI 8.4-9.7)。A、B和C三组的5年RFS率分别为77.8%、77.1% 和 85.8%,三组间没有统计学差异(log rank P=0.162)。C组较A组有获益倾向(HR =0.44, 95% CI 0.18-1.05)。A+B组的5年RFS率为77.5% ,C组的为85.8% (HR= 0.52,95% CI 0.23-1.15; log-rank P=0.102)。ER状态不影响5年RFS率(ER阳性患者5年RFS为79.8%,ER阴性的为81.1%; HR=1.032, 95% CI 0.50-2.11; log-rank P= 0.932)。A组和C组的OS没有统计学差异(HR=1.00, 95% CI 0.31-3.27)。
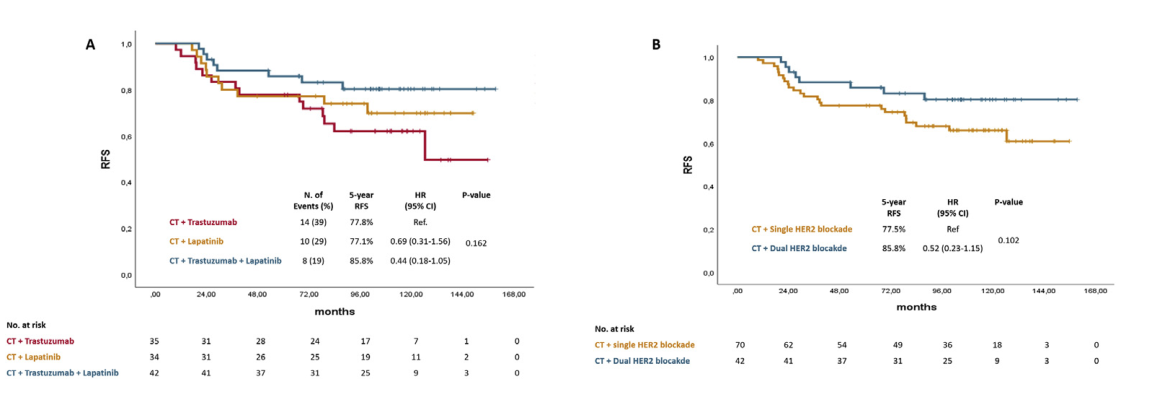
RFS比较
获得pCR的患者5年RFS率较没有pCR患者的高(97.3% vs 72.7%,HR=0.12, 95% CI 0.03-0.49; log-rank P < 0.001)。ER阴性患者 (pCR vs no-pCR: 94.7% vs 69.2%, HR 0.11, 95% CI 0.01-0.85; log-rank P=0.010) 和ER阳性患者 (pCR vs no-pCR: 100% vs 74.5%, HR=0.12, 95% CI 0.02-0.90; log-rank P=0.014)也有类似结果。
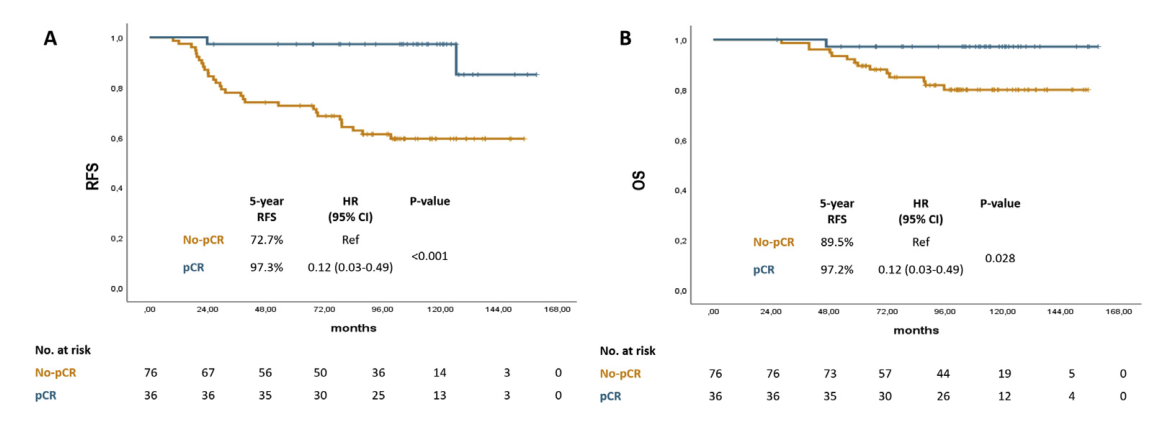
pCR分层的RFS和OS
同样,获得pCR的患者5年OS较没有pCR患者的高(97.2% vs 89.5%,HR=0.12, 95% CI 0.03-0.49; log-rank P= 0.028 )。
肿瘤浸润性淋巴细胞(TILs)跟RFS显著相关(HR=0.978为每增加1%含量TILs)。Luminal-A亚型是较好的RFS的独立预后因素(HR=0.29, 95% CI 0.09-0.94, p = 0.040)。
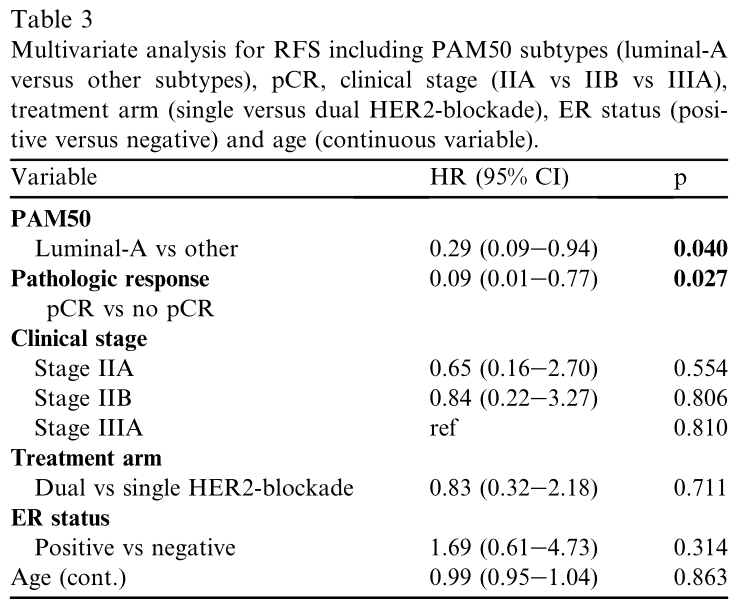
RFS预后因素
84例患者可进行PAM50亚型评估跟预后关系。其中HER2阳性为26.2% (N=22), luminal A 为25.0% (N =21), luminal B为 16.7% (N =14), basal- like为14.3% (N=12)和normal-like 为17.9% (N =15). 除去normal-like亚型患者, 各亚型患者的RFS没有统计学差异。多因素分析发现,PAM50分型 (luminal A vs 其他亚型)和pCR是独立预后因素。
综上,Cher-LOB研究生存分析证实pCR和TILs的预后作用,同时提示曲妥珠单抗联合拉帕替尼较曲妥珠单抗可改善患者预后倾向。
原始出处:
Guarneri V, Dieci MV, Griguolo G, et al. Trastuzumab-lapatinib as neoadjuvant therapy for HER2-positive early breast cancer: Survival analyses of the CHER-Lob trial. Eur J Cancer. 2021 Jun 18;153:133-141. doi: 10.1016/j.ejca.2021.05.018. Epub ahead of print. PMID: 34153715.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#曲妥珠#
30
#新辅助#
28
#拉帕替尼#
37
#乳腺癌患者#
38
谢谢分享
72
谢谢梅斯提供这么好的信息,学到很多
49