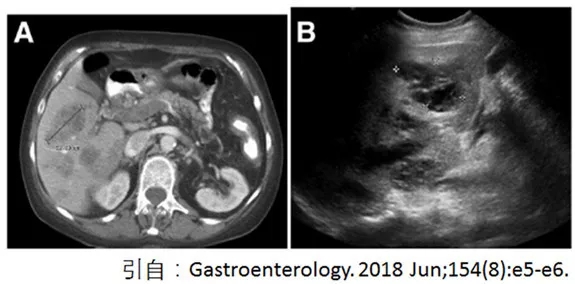
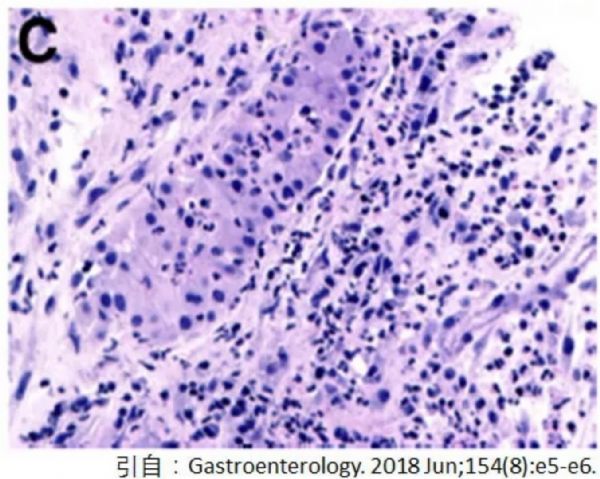
Gastroenterology:病例学习,炎症性肠病患者中的肝脏肿块
2018-06-17 鸟爪爪 IBD学术情报官 消化界
病例:一名74岁的女性患者,40岁时溃疡性结肠炎确诊,目前处于临床缓解期,使用英夫利西单抗维持治疗。3周前突然出现病情恶化,表现为腹泻和腹部不适。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gastroenterol#
28
#AST#
35
#GAS#
39
谢谢分享学习
71
谢谢分享学习
64
#肿块#
22
#Gastroenterology#
26
#炎症性#
26
#炎症性肠病患者#
20
学习了.长知识
71