Nucleic Acids Res:武大杜海宁课题组发现核蛋白在应急条件下的自噬降解新途径
2017-03-19 佚名 武汉大学生命科学学院
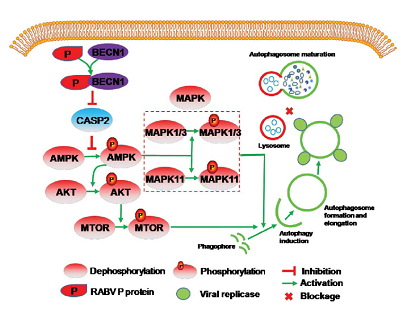
近日,国际著名学术期刊Nucleic Acids Research (IF:9.202)在线发表了武汉大学杜海宁课题组的最新研究成果。论文题目为“Gcn5-mediated Rph1 acetylation regulates its autophagic degradation under DNA Damage Stress”(乙酰转移酶Gcn5介导的乙酰化修饰调控组蛋白去甲基化酶Rph1在DN
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#核蛋白#
0
#acid#
0
#CID#
37
#新途径#
37