Aging Cell:APOE ε4携带者为什么是阿尔兹海默症的高风险人群?
2021-05-05 haibei MedSci原创
最近研究人员探究了APOE ε4基因型对阿尔茨海默病(AD)患者血小板和淋巴细胞代谢的影响。
载脂蛋白E(APOE)是散发性阿尔茨海默病(AD)最强的遗传风险因素。APOE有三种等位基因:ε2(降低AD风险),ε3(中性AD风险),和ε4(增加AD风险)。携带APOE ε4等位基因的人患AD的可能性是原来的三倍到四倍,而纯合子患AD的可能性是原来的十倍到十五倍。
统计数据显示,15%-25%的人口携带APOE ε4等位基因,2%-3%为纯合子。AD风险和APOE之间的确切机制尚不清楚,尽管有数据表明APOE ε4对线粒体的影响可能介导了这种关联。
APOE基因的产物是一种脂蛋白,其与脂质结合并在胆固醇代谢中发挥作用。在大脑中,APOE是主要的胆固醇携带蛋白,它主要由星形胶质细胞表达,并将胆固醇运送到神经元。压力条件也会导致神经元和小胶质细胞表达APOE。
最近研究人员探究了APOE ε4基因型对阿尔茨海默病(AD)患者血小板和淋巴细胞代谢的影响。结果显示,APOE ε4携带者的平均血小板线粒体细胞色素氧化酶Vmax活性较低,淋巴细胞Annexin V(一种细胞凋亡的标志物)明显较高。
此外,在APOE ε4的淋巴细胞中,介导有丝分裂和能量感应的蛋白质较高,这可能代表了补偿性变化,这也再现了在死后AD患者大脑中观察到的现象。
对脂质合成途径的分析发现,APOE ε4淋巴细胞的AceCSI、ATP CL和磷酸化的ACC水平更高。在死后的脑组织中也观察到淋巴细胞的ACC变化。
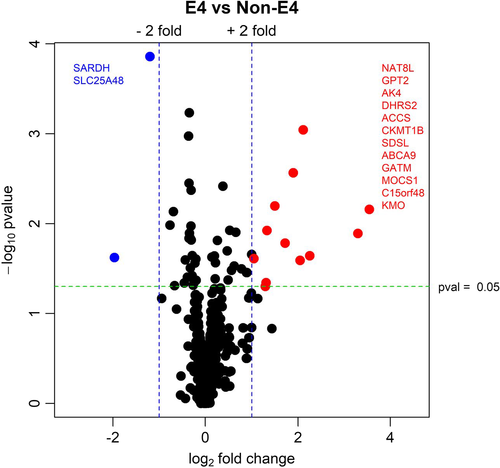
淋巴细胞的RNAseq MitoCarta3.0分析
淋巴细胞RNAseq数据显示,APOE ε4载体鞘磷脂转运体3(SPNS3)和整合素α亚单位1(ITGA1)的表达较低。RNAseq途径分析进一步显示,APOE ε4等位基因激活了炎症途径并调节了生物能量信号。这些发现支持APOE基因型和生物能量途径之间的关系,并表明APOE ε4携带者的血小板和淋巴细胞存在于生物能量的压力状态。
用药和脑部组织病理学都不能解释这些发现,这些发现定义了一个由APOE ε4决定的分子和系统表型,为AD病因学提供了依据。
原始出处:
Heather M. Wilkins et al. Bioenergetic and inflammatory systemic phenotypes in Alzheimer’s disease APOE ε4‐carriers. Aging Cell (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
34
#CEL#
36
#高风险#
23
#携带者#
46
#阿尔兹海默#
32
#APOE#
21
好文章!
64
用药和脑部组织病理学都不能解释这些发现,这些发现定义了一个由APOE ε4决定的分子和系统表型,为AD病因学提供了依据。
42
学习了
54