【1】Brit J Cancer:使用剪接寡核苷酸靶向ERG致瘤基因来治疗前列腺癌的研究
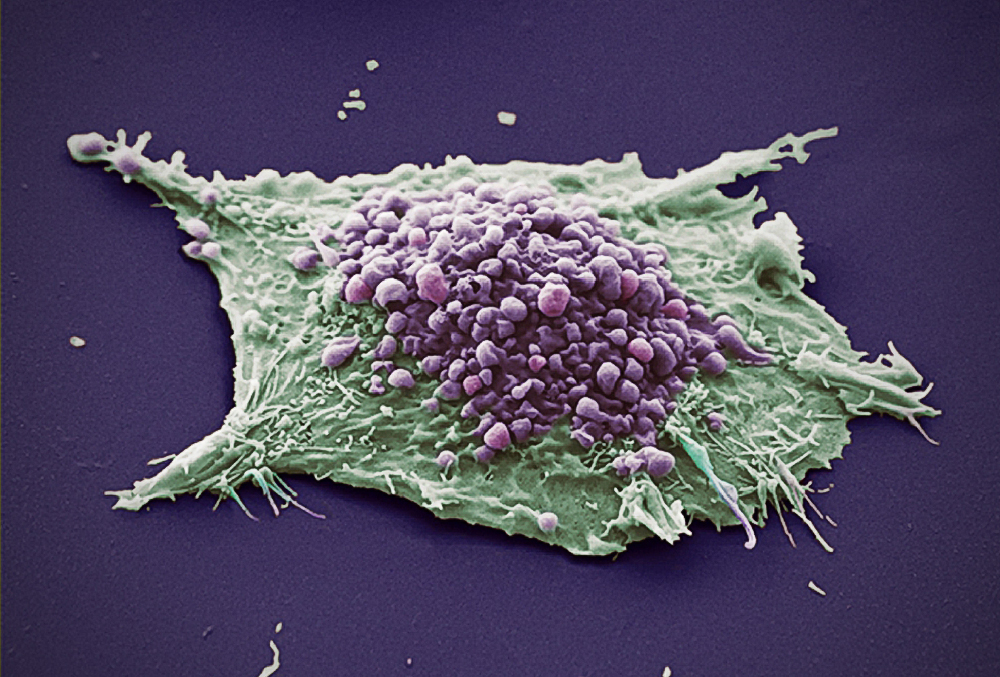
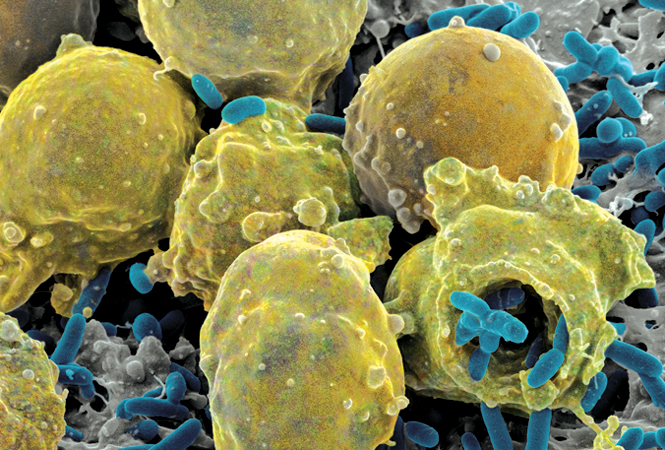
ERG致瘤基因是ETS转录因子家族的一个成员,是前列腺癌的遗传驱使因子。在50%的案例中通过与雄激素响应的TMPRSS2启动子融合被激活。因此,在开发靶向ERG的药物上研究较热。最近,有研究人员通过反义的方法,设计了一个基于吗啉代的寡核苷酸通过跳过第4外显子来靶向ERG。
研究发现,在VCaP细胞中,设计的2个剪接寡核苷酸(SSOs)在诱导第4外显子跳过中均有效。在单一的一次转染后,总的ERG蛋白水平减少持续时间高达96小时。SSO诱导的ERG减少能够减弱细胞增殖、细胞迁移和显著在增加细胞凋亡。研究人员还观察到了cyclin D1、c-Myc和Wnt信号通路成员catenin以及激活Wnt信号的标记p-LRP6蛋白水平均同时减少。研究人员在小鼠的MG63异种种植模型中测试了3'剪接位点SSO,发现肿瘤生长减少。研究人员还阐释了SSO的3'剪接位点能够在患者来源的前列腺癌组织中减少ERG的表达。
最后,研究人员指出,他们成功的设计和测试了基于吗啉代的SOs,能够ERG表达减少,从而进一步减少细胞增殖、细胞迁移和增加细胞凋亡。小鼠和人类前列腺癌样本测试表明了SSOs能够有效的靶向致瘤基因。因此,他们的研究鼓舞了人们需要进一步的在体内测试SSOs靶向ERG致瘤基因的效果。
【2】Brit J Cancer:前列腺癌积极监控,手术或者放疗的成本-效益分析比较
目前,局部前列腺癌治疗方法的成本-效益相关证据仍旧有限。最近,有研究人员在一个UK NHS前瞻性前列腺癌检测和治疗(ProtecT)随机对照试验中评估了积极监控,手术和放疗的成本-效果情况。该试验的随访时间均值为10年。
研究发现,调整后的质量调整生命年(QALYs)在积极监控组(6.89),放疗组(7.09)和手术组(6.91)相似。积极监控组比放疗组(7361英镑)和手术组(7519英镑)具有更低的调整后花费(5913英镑)。在UK NICE意愿支付阈值(每QALY为2万英镑)中,放疗很可能是性价比最高的选择(58%的可能性)。亚群分析确认了放疗是老年男性和中度/高风险疾病组划算的选择;积极监控对相对年轻的男性和低风险组是划算的选择。
最后,研究人员指出,还需要更长的随访和建模来确定男性前列腺癌最划算的选择。
【3】Prostate Cancer P D:放疗前列腺癌患者中高强度间歇训练与抗阻训练效果比较
运动训练对经历了放疗(RT)前列腺癌患者的放疗相关副作用控制方面具有有利的影响。然而,最优的训练计划还没有确定。最近,有研究人员进行了一个随即对照试验,在进行RT的PCa患者中调查了高强度的间歇性训练(HIIT)和抗阻训练(RES)与日常护理(UC)相比对癌症治疗相关疲劳(CTRF)(主要结果)的影响,也包括了对生活质量、抑郁、白天嗜睡、失眠、睡眠质量、功能锻炼能力和执行功能的影响。
研究人员经经历了RT的PCa患者(进行过或者没有进行过ADT治疗)随机分配到HIIT、RES和UC组。两种锻炼计划每周3次,进行5-8周。HIIT的间隔时间为8-15×60秒(最大心率≥85%);每个肌肉群分别进行1-3组,每组8-12次的RES训练。研究发现,共有72名受试者(69.1±8.2岁)完成了研究。没有发生与运动相关的副作用事件。与UC相比,HIIT(p=0.012)和RES(p=0.039)训练减弱了CTRF的增加。与UC相比(+0.1%),6分钟行走测试的功能锻炼能力在HIIT和RES后增加(p分别为0.043和0.041)。另外,两组之间的其他次要变量没有差异。
最后,研究人员指出,两种锻炼方法均表现出了对CTRF和功能锻炼能力益处。另外,HIIT和RES都很安全且参与率高。
【4】Prostate Cancer P D:较少的经尿道系统活检核心能否与磁共振成像/超声融合活检具有相同的前列腺癌检出率?
随着活检核心数目的增加,不舒适和并发症的发生率也随着增加。在许多研究中,前列腺癌活检的方法已经由系统生物活检(SB)和靶向生物活检(TB)得到了改善。然而,能够平衡活检并发症和活检准确率的最优前列腺取样方法仍旧不明确。最近,有研究人员探索了一种最优的前列腺癌(PCa)取样方法,且具有更少的SB核心数目。
研究前瞻性的招募了前列腺成像报告至少有1个病变部位和数据系统≥3的患者。每位患者均进行了TB和SB作为参照。假定的取样方案包括TB、SB和TB+nSB(非靶向区域活检)。研究发现,在165名患者中,107名(64.8%)患者诊断为PCa,91名(55.2%)患者通过TB+SB诊断为csPCa。在PCa和csPCa患者中,核磁共振成像(MRI)的真阴性案例比例分别为50.5%(54例)和例46.2%(42例),非靶向区域活检的假阴性比例分别为49.5%(53例)和53.8%(49例)。阳性活检案例中的最大癌症比例在这些真假队列中差异显著。而在PCa或csPCa的检出方面,TB+nSB和TB+SB没有差异。
最后,研究人员指出,最优的取样方法为TB+nSB,且具有更少的SB核心数目。该方法与标准的TB+SB联用MRI/超声融合活检的检出率相同。
【5】Modern Pathology:根治性前列腺切除术中的筛状结构能够预测肿瘤结果
前列腺癌患者中,格林森评分是临床结果的一个重要参数。格林森评分8是一种异质性疾病,包括了格林森3+5、4+4和5+3肿瘤,并涵盖了很大范围的肿瘤生长模式。
最近,有研究人员描述了个体生长模式,并鉴定了格林森评分8前列腺癌患者的预后参数。研究人员分析了1064个根治性前列腺切除样本,记录了个体格林森4和5的生长模式以及导管内癌的存在,并评估生化复发和无转移生存情况。研究发现,140名(13%)患者为格林森评分8,其中76名(54%)为格林森评分3+5,46名(33%)为4+4,18名(13%)为5+3。在格林森评分为4+4的患者中,侵袭性筛状癌和/或导管内癌(n=87,62%)中的发生率率要比3+5 (47%;P<0.001)患者和5+3 (44%;P<0.001)患者更高。110名男性中为格林森模式5:99个案例中为单细胞和/或索状(90%),32个案例中为实体场(29%)。实体场模式5与筛状结果的共存频率(23/32, 72%)要比非实体场模式(36/78, 46%, P=0.02)更高。在包括年龄、前列腺特异性抗原、pT-阶段、手术切缘和淋巴结转移的多变量分析中,筛状结构是无生化复发(HR 2.0, 95%CI 1.0-3.7; P=0.04)和无转移(HR 3.5, 95%CI 1.0-12.3; P=0.05)的一个独立参数。
最后,研究人员指出,侵袭性筛状癌和/或导管内癌在格林森4+4前列腺癌患者中要比格林森3+5和5+3患者的比例更高,并且是生化复发和转移的一个独立参数。因此,筛状结构有助于格林森评分8前列腺癌患者的风险分层。
【6】Sci Rep:不同程度肥胖患者根治性前列腺切除术后生化复发的风险因子差异分析
最近,有研究人员评估了通过肥胖程度分层的患者中,在根治性前列腺切除术后生化复发(BCR)风险因子的差异情况,并关注了使用的手术方法。
研究包括了来自2个医疗中心的经历了根治性前列腺切除术的3099名患者,时间为2008年到2018年。研究人员将这些患者根据身体质量指数(BMI)进行分组:正常组、超重组和肥胖组。研究发现,肥胖组和超重组中分别包括378名(12.2%)患者和1815名(58.6%)患者。同时,1324名患者经历了耻骨后前列腺切除(RRP),1775名患者经历了机器人辅助的腹腔镜前列腺切除术(RALP)。多变量分析表明在超重组和肥胖组中,经历了RALP的患者比经历了RRP的患者具有显著更低的无生存BCR(风险比分别为0.75(95%CI 0.59-0.95, p=0.01和0.55(95%CI 0.33-0.90, p=0.02)。
最后,研究人员指出,肥胖的程度与无生存BCR物直接相关性。在超重组和肥胖组中,机器人前列腺切除术的无生存BCR要比开放式前列腺切除更好。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#期前列腺癌#
39
学习了
71
还
110
前列腺癌相关研究,学习了,谢谢梅斯
58
好文章
105
学习了
101
很好,希望继续有这样的文章
87