Lancet Oncol:杜鲁伐单抗联合立体定向放疗明显改善早期NSCLC患者预后
2021-05-19 Nebula MedSci原创
杜鲁伐单抗新辅助治疗联合立体定向放疗的耐受性良好,安全性高,且可提高早期NSCLC患者的主要病理缓解率
既往关于新辅助抗PD-1或抗PD-L1单药治疗早期非小细胞肺癌的2期试验报道,主要病理缓解率浮动在15%-45%。有证据提示,立体定向放射疗法可能是晚期非小细胞肺癌(NSCLC)的有效免疫调节剂。
本研究旨在评估在早期NSCLC患者中使用立体定向放射疗法作为免疫调节剂,以增强与抗PD-L1抗体杜鲁伐单抗相关的抗肿瘤免疫应答的效果。
这是一项单中心、开放标签的、随机对照的2期试验,对比了新辅助杜鲁伐单抗单药治疗和联合立体定向放疗用于早期NSCLC患者的疗效和安全性。招募了可手术切除的早期NSCLC患者,1:1随机分至两组。主要终点是主要病理缓解率。
2017年1月25日-2020年9月15日,共筛选了96位患者,其中60位被随机分至杜鲁伐单抗单药组或杜鲁伐单抗联合放疗组(各30位)。每组30位患者中均有26位(87%)进行了手术切除肿瘤。
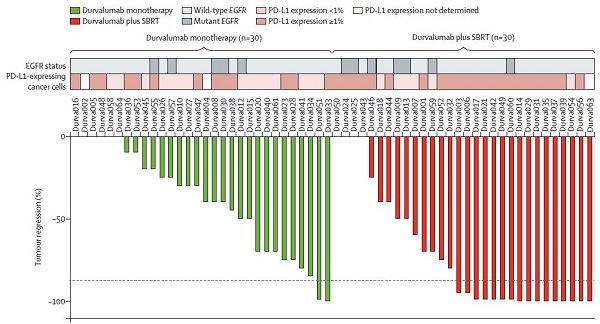
肿瘤消退的瀑布图
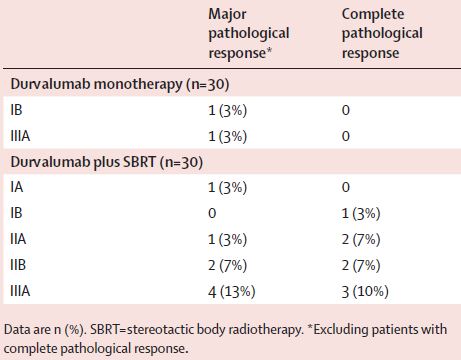
杜鲁伐单抗单药组有两位患者获得了主要病理缓解(6.7%,95%CI 0.8-22.1),而联合组有16位患者获得了主要病理缓解(53.3%,95%CI 3.2-79.6;p<0.0001)。两组之间的主要病理缓解率差异显着(粗略优势比 16.0, 95% CI 3.2–79.6; p<0.0001)。在联合组获得主要病理缓解的16位患者中,有8位(50%)为完全病理缓解。
主要和完全病理缓解情况
联合组有3位(10%)患者因免疫相关不良事件撤销了第二疗程的杜鲁伐单抗。杜鲁伐单抗单药组有5位(17%)患者发生了3-4级不良反应,联合组有6位(20%)。
不良反应
最常见的3-4级不良事件有低钠血症(单药组 10%)和高脂血症(联合组 10%)。两组各有两位患者发生了重度不良反应(单药组一例肺栓塞和一例卒中;联合组一例胰腺炎和一例疲劳)。无治疗相关死亡。
综上所述,杜鲁伐单抗新辅助治疗联合立体定向放疗的耐受性良好,安全性高,且可提高早期NSCLC患者的主要病理缓解率。应开展更大规模的试验验证该治疗策略。
原始出处:
Nasser K Altorki, et al. Neoadjuvant durvalumab with or without stereotactic body radiotherapy in patients with early-stage non-small-cell lung cancer: a single-centre, randomised phase 2 trial. The Lancet Oncology. May 17, 2021. https://doi.org/10.1016/S1470-2045(21)00149-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
32
#患者预后#
35
#Lancet#
26
#立体定向#
0
#SCLC患者#
31
#定向#
44
#NSCLC患者#
29
#立体定向放疗#
51
顶刊就是不一样,质量很高,内容精彩!学到很多
61
谢谢梅斯分享这么多精彩信息
47