J Thorac Oncol:纳米-紫杉醇 vs 多西他赛治疗晚期NSCLC患者的疗效
2021-05-01 Nebula MedSci原创
对于既往治疗过的晚期NSCLC患者,在总生存期方面,nab-紫杉醇的疗效并不劣于多西他赛。nab-紫杉醇或可成为这类患者的一种标准治疗选择
全球非小细胞肺癌(NSCLC)高发,而且相关死亡率居高不下。对驱动恶性肿瘤进行的分子通路的了解可推进分子靶向药的发展,从而提高携带相应遗传变异的NSCLC患者的预后。
本研究旨在评估纳米颗粒包裹(nab-)紫杉醇用于既往治疗过的晚期NSCLC患者的疗效和安全性。
这是一项随机、开放标签的非劣效性3期试验,招募了既往采用细胞毒性化疗治疗过的晚期NSCLC患者,1:1随机分至两组,接受多西他赛(60 mg/m2;第1天)或nab-紫杉醇(100 mg/m2,第1、8和15天)治疗,21天一疗程。主要终点是意向治疗人群中的总生存期。
2015年5月22日-2018年3月12日,共有503位患者随机分至治疗组:nab-紫杉醇组 252位、多西他赛组 251位。
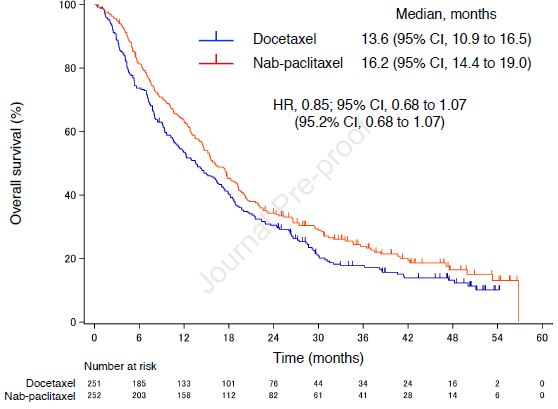
总生存期
nab-紫杉醇组和多西他赛组的中位总生存期分别为16.2个月(95% CI 10.9-19.0)和13.6个月(95% CI 10.9-16.5;HR 0.85, 95% CI 0.68-1.07)。
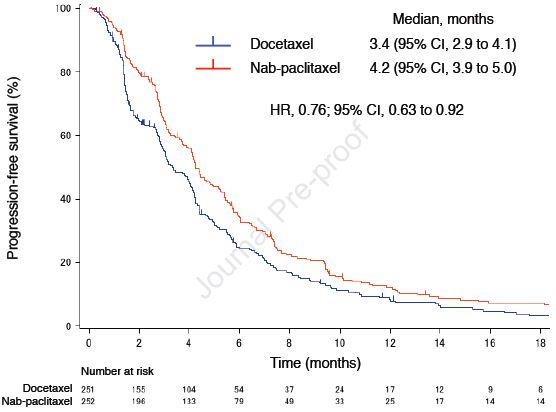
无进展生存期
nab-紫杉醇组和多西他赛组的中位无进展生存期分别是4.2个月(95% CI 3.9-5.0)和3.4个月(95% CI 2.9-4.1;HR 0.76, 95% CI 0.63-0.92;p=0.0042)。nab-紫杉醇组和多西他赛组的客观缓解率分别为29.9%(95% CI 24.0-36.2)和15.4%(95% CI 10.9-20.7;p=0.0002),而且无论肿瘤组织类型如何,nab-紫杉醇都可相比多西他赛显著改善NSCLC患者的预后。
两组最常见的≥3级的不良反应有发热性中性粒细胞减少症(nab-紫杉醇组 vs 多西他赛组:2% vs 22%)和外周感觉神经病变(10% vs 1%)。
综上,对于既往治疗过的晚期NSCLC患者,在总生存期方面,nab-紫杉醇的疗效并不劣于多西他赛。nab-紫杉醇或可成为这类患者的一种标准治疗选择。
原始出处:
Yoneshima Yasuto,Morita Satoshi,Ando Masahiko et al. Phase 3 trial comparing nab-paclitaxel with docetaxel for previously treated advanced non-small cell lung cancer. J Thorac Oncol, 2021, https://doi.org/10.1016/j.jtho.2021.03.027
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
42
#SCLC患者#
42
#THORAC#
32
#NSCLC患者#
33
#晚期NSCLC#
30
精彩评论,需要您登录查看
71
谢谢梅斯提供这么好的信息,学到很多
52
JTO上有很多不错的好文章,谢谢梅斯及时上新
54
谢谢梅斯分享这么多精彩信息
43
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
45