Lancet Oncol:新亚型!HER2弱阳性乳腺癌的临床和分子特征
2021-07-12 MedSci原创 MedSci原创
HER2-弱阳性肿瘤可通过标准化IHC确定为乳腺癌的新亚组,区别于HER2-零肿瘤
抗HER2抗体-药物偶联物的开发为包括HER2低表达患者在内的乳腺癌患者开辟了新的治疗选择。为了表征这种新的乳腺癌亚型,Denkert等人比较了HER2-弱阳性和HER2-零乳腺癌的临床和分子特征,包括对新辅助化疗的反应和预后。
在本次对个体患者数据的汇总分析系中,研究人员评估了2012年7月30日-2019年3月20日期间四项前瞻性新辅助临床试验中的采用新辅助联合化疗的2310位HER2非扩增型原发性乳腺癌患者队列。所有试验患者在随机分组前都进行了HER2检测。HER2弱阳性状态定义为免疫组化(IHC)1+或2+/原位杂交阴性,HER2-零定义为IHC0。1694位患者中位随访了46.6个月(IQR 35.0-52.3),可进行无病生存期和总生存期评估。
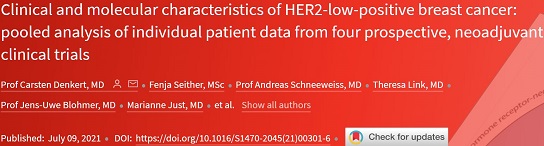
根据激素受体和HER2表达情况进行乳腺癌分类
在2310例肿瘤中,1098例(47.5%)为HER2弱阳性,1212例(52.5%)为HER2-零。1098例HER2弱阳性肿瘤中有703例(64.0%)为激素受体阳性,相比之下,1212例HER2-零肿瘤中仅有445例(36.7%)为激素受体阳性(p<0.0001)。HER2弱阳性肿瘤的病理完全缓解率明显低于HER2-零肿瘤(29.2% vs 39.0%, p=0.0002)。与激素受体阳性亚组中,与HER2-零肿瘤相比,HER2-弱阳性肿瘤的病理完全缓解也显著降低(17.5% vs 23.6%,p<0.024),但在激素受体阴性亚组中,无此差异(50.1% vs 48.0%,p=0.21)。
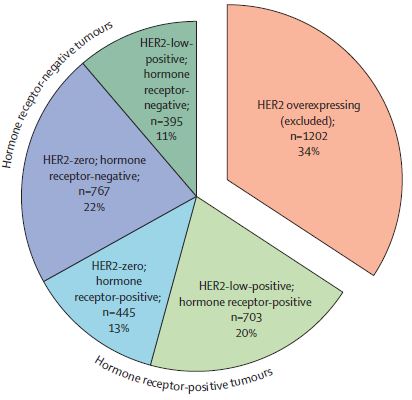
各分组的生存预后
HER2-弱阳性肿瘤患者的生存期明显长于HER2-零肿瘤患者(3年无病生存率:83.4% vs 76.1%,p=0.0084;3年总生存率:91.6% vs 85.8%,p=0.0016)。在激素受体阴性肿瘤患者中也观察到了类似的生存差异(3年无病生存率:90.2% vs 84.3%,p=0.0016;3年总生存率:91.6% vs 85.8%,p=0.0016),但在激素受体阳性肿瘤患者中无此差异。
综上所述,HER2-弱阳性肿瘤可通过标准化IHC确定为乳腺癌的新亚组,区别于HER2-零肿瘤。HER2-弱阳性肿瘤具有特定的生物学特性,对治疗的反应和预后表现出差异,这与治疗耐药、激素受体阴性的肿瘤尤其相关。该研究结果为更好地了解乳腺癌亚型的生物学和完善未来的诊疗策略提供了基础。
原始出处:
Carsten Denkert, et al. Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. The Lancet Oncology. July 09, 2021. https://doi.org/10.1016/S1470-2045(21)00301-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#弱阳性#
29
#分子特征#
42
#Lancet#
35
#Oncol#
38
顶刊就是不一样,质量很高,内容精彩!学到很多
62
谢谢梅斯分享这么多精彩信息
54
IHC 1-2个+
58