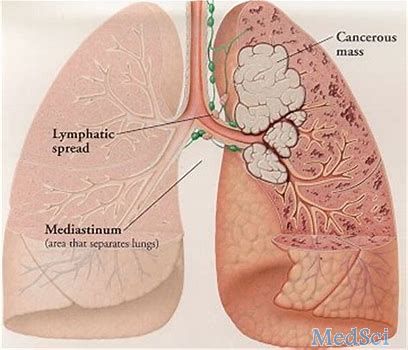
2018年WCLC:Atezolizumab治疗IV期非鳞状非小细胞肺癌的有效性和安全性
2018-09-28 MedSci MedSci原创
在第19届世界肺癌大会(WCLC)上,III期临床试验(IMpower132试验)的中期结果正式公布,Atezolizumab在治疗IV期非鳞状非小细胞肺癌(NSCLC)方面表现出积极的有效性和安全性。
在第19届世界肺癌大会(WCLC)上,III期临床试验(IMpower132试验)的中期结果正式公布,Atezolizumab在治疗IV期非鳞状非小细胞肺癌(NSCLC)方面表现出积极的有效性和安全性。该试验评估了Atezolizumab联合培美曲塞、卡铂或顺铂对无进展生存期(PFS)和总生存期(OS)的影响。
德克萨斯大学安德森癌症中心医学博士Vassiliki A. Papadimitrakopoulou说:“IMpower132在意向治疗人群中实现了它的主要终点。Atezolizumab联合培美曲塞、卡铂或顺铂的疗法具有可控的安全性,符合各种已知的安全标准”。Papadimitrakopoulou博士及其同事将患有IV期非鳞状NSCLC的患者(n = 578)随机分组接受4或6个周期的卡铂或顺铂以及培美曲塞(500 mg/ m2)治疗(PP组,n = 286)或这些药物与Atezolizumab联合使用(APP组,n = 292)。该治疗阶段完成之后是维持期,其中PP组使用的是培美曲塞维持治疗,APP组使用的是Atezolizumab+培美曲塞维持治疗。
原始出处:
http://www.firstwordpharma.com/node/1593505#axzz5SJBcSQbc
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
38
#mAb#
23
#非鳞状非小细胞肺癌#
35
#WCLC#
23