JAMA:快速静脉输液对接受气管插管的危重症患者心血管衰竭风险的影响
2022-06-23 zhangfan MedSci原创
对于接受气管插管的危重症患者,快速静脉输液不能降低患者严重低血压、心脏骤停或死亡风险。
2014-2018年,美国每年约有200万危重症成人患者接受气管插管治疗。重症监护病房(ICU)患者中,25%-40%的气管插管患者出现低血压,可导致心脏骤停或死亡。气管插管期间的低血压,部分原因是药物诱导的血管舒张和正压通气导致胸内压力增加引起静脉血返回心脏的能力下降。静脉输液可通过短暂增加血容量来抵消上述影响。近日研究人员考察了在接受气管插管的危重成人患者中,手术期间或术后不久,快速静脉输液对患者严重低血压、心脏骤停或死亡风险的影响。

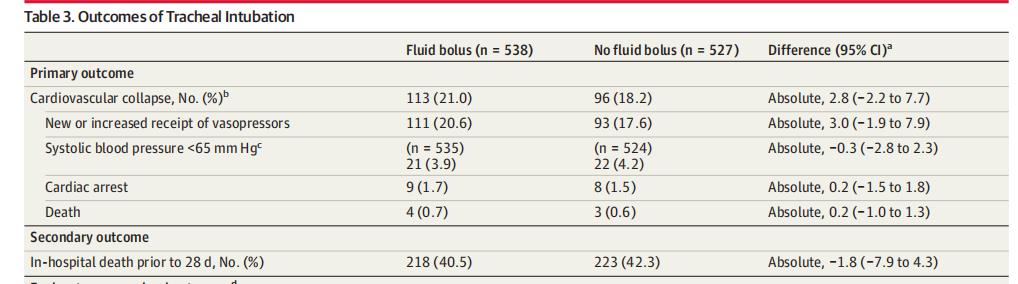
本次研究在美国11个重症监护病房开展,1067名接受镇静气管插管和正压通气的危重患者参与研究,随机接受500-mL静脉输液(n=538)或不输液(n=527)。研究的主要终点为心血管衰竭,定义为在麻醉诱导至气管插管后2分钟之间新接受或增加血管升压药或收缩压<65mmHg,或麻醉诱导至气管插管后1小时之间心脏骤停或死亡。次要结果是28天内死亡。
1065例(99.8%)患者完成研究,平均年龄62岁,42.1%为女性。输液组113例(21.0%)患者出现心血管衰竭,未输液组96例(18.2%,绝对差异2.8%)。未输液组17.6%的患者新或增加使用血管升压药,输液组20.6%;出现收缩压低于65 mm Hg的患者比例分别为3.9%和4.2%;心脏骤停发生率分别为1.7%和1.5%,死亡率分别为0.7%和0.6%。输液组218例(40.5%)患者28天内死亡,未输液组为223例(42.3%,绝对差异−1.8%)。
研究认为,对于接受气管插管的危重症患者,快速静脉输液不能降低患者严重低血压、心脏骤停或死亡风险。
原始出处:
Derek W. Russell et al. Effect of Fluid Bolus Administration on Cardiovascular Collapse Among Critically Ill Patients Undergoing Tracheal Intubation A Randomized Clinical Trial. JAMA,16 June 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#静脉#
46
#重症患者#
43
#静脉输液#
42
#气管插管#
52
#危重症患者#
52
JAMA上文章都是顶级的,谢谢梅斯及时上新
26