Bipolar Disord:卡利拉嗪治疗双相I型抑郁症的疗效和安全性
2021-05-07 MedSci原创 MedSci原创
有症状的双相情感障碍患者中,抑郁症发作的频率是躁狂症发作的三倍,在病程中较早出现,并在病程后期成为主要的情绪状态。卡利拉嗪被FDA批准用于治疗成人精神分裂症以及与双相情感障碍相关的急性躁狂、急性混合或
有症状的双相情感障碍患者中,抑郁症发作的频率是躁狂症发作的三倍,在病程中较早出现,并在病程后期成为主要的情绪状态。卡利拉嗪被FDA批准用于治疗成人精神分裂症以及与双相情感障碍相关的急性躁狂、急性混合或抑郁发作,并正在研究用于治疗严重抑郁症。近日,一项3期双盲安慰剂对照研究中研究人员评估了卡利拉嗪治疗成人双相情感障碍抑郁期的疗效、安全性和耐受性,研究结果已发表于Bipolar Disord。
研究纳入了 167名双相I型障碍和当前抑郁症发作的成年患者,随机分配到安慰剂、卡利拉嗪 1.5mg/天(n = 168)或卡利拉嗪3.0mg/天(n = 158)。研究结果是与安慰剂相比,从基线到第6周,蒙哥马利-奥斯伯格抑郁症评定量表(MADRS)总分(主要)和临床全球印象-严重程度(CGI-S)得分(次要)的变化。监测不良事件(AEs)、实验室结果、生命体征和自杀风险。
结果显示,与安慰剂相比,1.5mg/天的卡利拉嗪可明显减少初级(MADRS LSMD = -2.5;校正后P = .0417)和次级(CGI-S LSMD = -0.3;校正后P = .0417)疗效参数上的抑郁症状;卡利拉嗪3.0mg/天的差异无统计学意义。常见的治疗突发AE(在任何一组中≥5%,至少是安慰剂的两倍)是失神症、不安、恶心和疲劳。各组的平均代谢参数变化不大,具有可比性;所有组的平均体重增加≤0.5公斤。
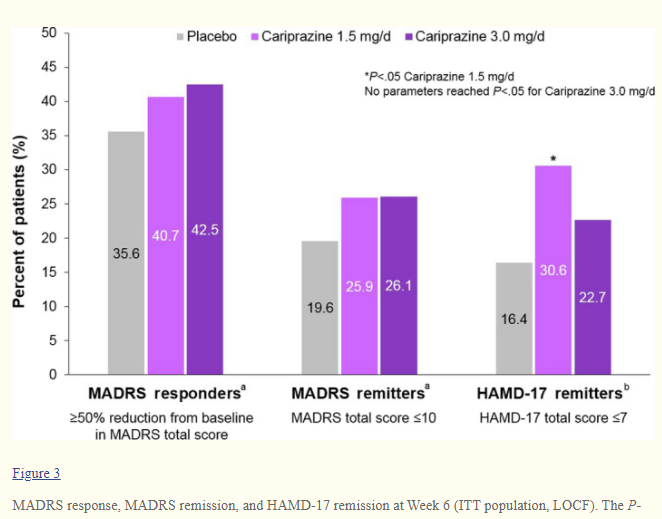
综上所述,该研究结果表明,与安慰剂相比,1.5mg/天的卡利拉嗪可明显减少成人双相I型抑郁症患者的抑郁症状,但3.0mg/天的卡利拉嗪的差异不大。安全性和耐受性情况与以前对卡利拉嗪的研究相似。
原始出处:
Willie R Earley, et al., Efficacy and safety of cariprazine in bipolar I depression: A double-blind, placebo-controlled phase 3 study. Bipolar Disord. 2020 Jun;22(4):372-384. doi: 10.1111/bdi.12852.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Dis#
15
#疗效和安全性#
29
#Disord#
30
#IPO#
0
谢谢梅斯提供这么好的信息,学到很多
36