重磅!第一个PD-L1抑制剂获得转移期NSCLC适应症
2016-10-20 王鑫 肿瘤资讯
今天,罗氏(Roche)集团旗下基因泰克(Genentech)公司宣布,美国FDA批准其免疫疗法药物atezolizumab用于治疗转移性非小细胞肺癌(NSCLC)。atezolizumab治疗转移期肺癌的III期临床实验结果于10月9日在ESMO大会上公布,让我们来看看这项研究的具体内容吧!2016年10月9日来自法国的马赛大学的Fabrice Barlesi教授在ESMO大会上口头报告PD-L
今天,罗氏(Roche)集团旗下基因泰克(Genentech)公司宣布,美国FDA批准其免疫疗法药物atezolizumab用于治疗转移性非小细胞肺癌(NSCLC)。atezolizumab治疗转移期肺癌的III期临床实验结果于10月9日在ESMO大会上公布,让我们来看看这项研究的具体内容吧!
2016年10月9日来自法国的马赛大学的Fabrice Barlesi教授在ESMO大会上口头报告PD-L1抑制剂atezolizumab(atezo)对比多西他赛二、三线治疗NSCLC的随机Ⅲ期的OAK研究。证实atezo可显著延长OS,且生存获益与PD-L1表达水平和组织学类型无关,另外atezo毒性更低。
背景:
Atezo是一种人源化抗PD-L1单克隆抗体 与受体PD-1和B7.1结合,恢复肿瘤特异性T细胞功能。Ⅱ期POPLAR研究证明Atezo较多西他赛((doc)可能延长生存。该Ⅲ期、随机OAK研究比较Atezo和doc治疗既往治疗过NSCLC的疗效。
方法:
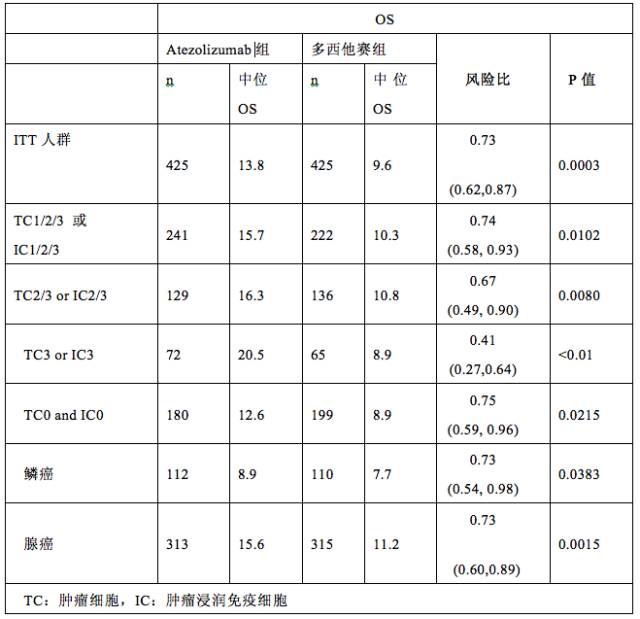
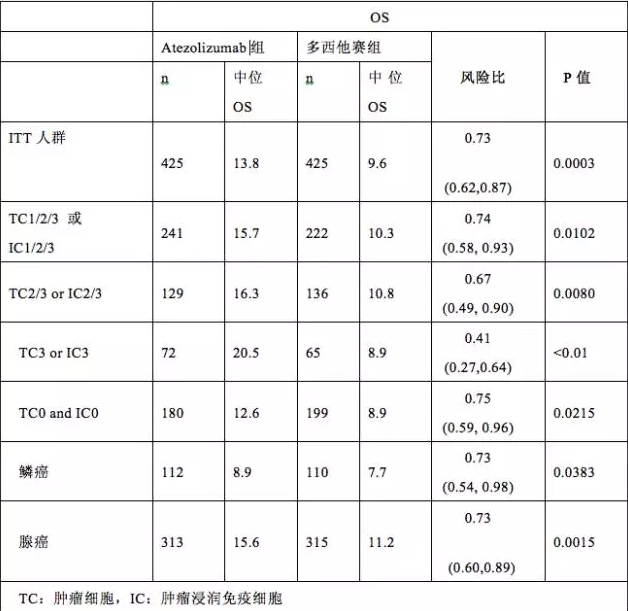
纳入既往治疗过的NSCLC患者。分层因素为:PD-L1表达状态、既往化疗方案(1线对比2线)、组织学类型。1:1随机分入atezo组 (1200 mg IV q3w) 或者 doc租 (75 mg/m2 IV q3w)。共同首要研究终点:ITT人群的OS,PD-L1表达肿瘤细胞(TC) 1/2/3亚组或肿瘤浸润免疫细胞(IC) 1/2/3亚组的OS。次要研究终点为PFS, ORR, DoR和安全性。
结果:
本次公布1225例患者中前期入组850例的数据。中位年龄64岁,61%男性,25%接受二线化疗,26%鳞癌,67%既往吸烟,37%PS评分为0。与doc组比较,Atezo组OS由9.6个月显著延长至13.8个月,死亡风险下降27%(HR 0.73; P = .0003)。在PD-L1表达TC1/2/3 或IC1/2/3亚组死亡风险下降26%(HR 0.74; P = .0102)。任何PD-L1表达水平OS均有获益,包括PD-L1表达TC0和IC0患者。PL-1高表达(TC3或 IC3)获益更加明显。鳞癌或非鳞癌均有生存获益。ITT人群,PFS的HR为0.95(2.8 个月对比 4.0个月),ORR13.6%对比13.4% ,DoR 16.3个月对比 6.2个月。atezo组3~4级治疗为15%,doc组为43%。atezo组无1例治疗相关死亡,而doc组1例。未发现新的AE。
结论:
这是第一个PD-L1抑制剂治疗NSCLC的Ⅲ期研究,证实较多西他赛,atezo二、三线治疗NSCLC显著延长OS,获益与组织学类型和PD-L1表达水平无关。Atezo较多西他赛安全性更高和耐受性更好。
专家点评:
主要研究者Barlesi教授指出,atezolizumab在不同瘤种中发挥作用。第一次报道OAK研究结果,初步分析1225例患者中850例生存和安全性数据,发现atezo显著降低死亡风险27%(p=0.0003),且与PD-L1表达水平无关,在PD-L1表达<1%患者仍然看到生存获益,但在PD-L1高表达患者死亡风险下降更明显为59%。这是第一个PD-L1药物的大型Ⅲ期研究,研究结果与Ⅱ期的POPLAR数据一致。Atezo为NSCLC提供新的二线治疗选择。
德国Gross hansdorf胸部肿瘤科Martin Reck教授评论说:PD-L1/PD-1抗体在NSCLC治疗中发挥越来越重要作用。OAK研究与POPLAR 和 CHECKMATE研究均显示出免疫治疗在延长生存方面的优势。值得注意是,该研究结果为OS的延长,甚至在PD-L1不表达患者中,说明PD-L1阴性不是免疫治疗排除的标准。PD-L1不是理想的疗效预测替代指标,只能作为有利因素,还需要新的标志物指导那类患者能从免疫治疗中真正获益。
Atezo是可与PD-L1蛋白相结合的单克隆抗体,当它结合肿瘤细胞和肿瘤浸润免疫细胞中表达的PD-L1时,可同时阻断该表面分子与PD-1受体以及B7.1受体之间的相互作用。通过抑制PD-L1的功能,Atezo可以活化T细胞的免疫应答来攻击癌细胞。目前,Atezo是FDA批准的第一个,也是唯一一个抗PD-L1的肿瘤免疫疗法。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PD-L1抑制剂#
27
#抑制剂#
25
#PD-L1#
37
#适应症#
38
#重磅#
25
厉害,希望尽快进入临床,拯救更多人
61