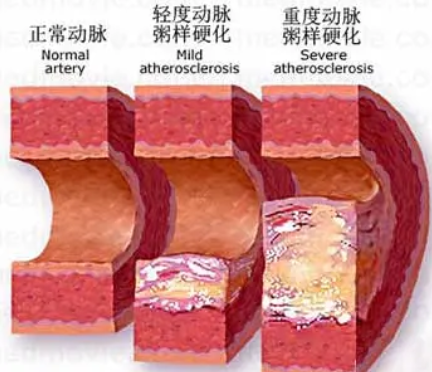
Hypertension:主动脉根部直径与动脉硬化
2021-10-11 MedSci原创 MedSci原创
较高的中心脉压与较高的颈股脉搏波速度(CFPWV)与心血管疾病(CVD)风险增加有关。男性与女性的较小与较大AoR的预后意义不同。
较高的中心脉压与较高的颈股脉搏波速度(CFPWV)与心血管疾病(CVD)风险增加有关。较小的主动脉根部直径(AoR)与较高的中心脉压有关。
近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员假设较小的AoR联合较高的CFPWV与CVD风险增加相关(相对于较大的AoR和较低的CFPWV)。
研究人员在基于社区的弗雷明汉研究(N=1970,平均年龄为60岁,57%为女性)中检验了这一假设。研究人员将参与者分为较小和较大的AoR组,并根据参与者的AoR变化轨迹和CFPWV(按性别中位数进行分类)对参与者进行了交叉分类。
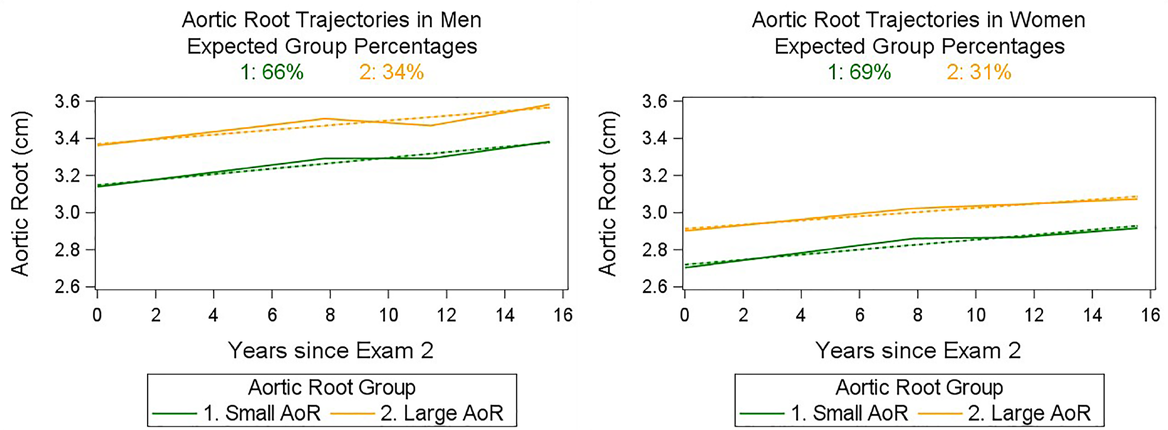
研究人员使用Cox回归将交叉分类组与随访(中位17年)期间的CVD发生率相关联:较低的CFPWV,较大的AoR(对照组;6.4/1000人每年);较低的CFPWV,较小的AoR(6.9/1000人每年);较高的CFPWV,较大的AoR(23.1/1000人每年);和较高的CFPWV,较小的AoR(21.9/1000人每年)。在性别汇总分析中,无论AoR大小如何,具有较高CFPWV个体经多变量调整的CVD风险增加1.8倍(P<0.01)。研究人员观察到了性别效应的改变(性别×AoR-CFPWV组交互作用的P=0.04)。在男性中,具有较小AoR和较高CFPWV个体CVD风险增加2.5至2.8倍(P<0.001)。在女性中,具有较大AoR和较高CFPWV个体CVD风险增加了70%至80%,但无统计学意义。
该研究的结果表明,男性与女性的较小与较大AoR的预后意义不同。需要额外的研究来证实这一结果。
原始出处:
Ramachandran S. Vasan.et al.Aortic Root Diameter and Arterial Stiffness: Conjoint Relations to the Incidence of Cardiovascular Disease in the Framingham Heart Study.Hypertension.2021.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.121.17702
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
24
#动脉硬化#
67
#TENS#
25
#主动脉#
40
#Hypertension#
40
气Fox垃圾人呢虚空间了没啊啊啊
65