CLEAR柯丽尔每日一例:食管裂孔疝、肝硬化伴胃及腹水疝入胸腔
2022-09-10 放射沙龙 放射沙龙
食管裂孔疝是由于食管裂空处先天发育不良或某些继发因素,所导致的腹压增高,导致膈食管裂孔部变松弛,腹腔内脏器通过食管裂孔进入胸腔。
【病例介绍】:
患者,女性,53岁,因肝硬化、腹水就诊,入院胸片示胸腔内右下缘可见一约6.5Cm之类圆形软组织肿块影,内密度欠均匀、边界尚清晰,随行上消化道造影显示(图1、2、3)心影后下缘膈肌上方可见一“类圆形”密度影,吞钡后显示胃底大部,胃粘膜影位于胸腔内,其后缘可见“环形”稍低密度影包绕,肿块影与心脏波动无同步。
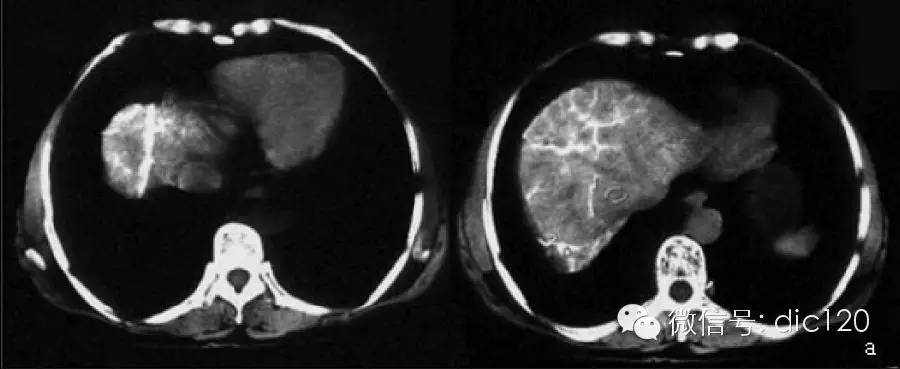
胸部CT检查显示(图4~11):心影后缘脊柱右前方见囊状肿块影,其向下层面可见囊状结构与膈下的胃体相连接,内密度不均、可见胃粘膜影位于肿块中心,周边见液体密度影环绕;肝脏形态缩小、比例失调,并可见多发不规则再生结节影出现,肝组织密度欠均匀,肝周包膜下可见液体密度影包绕;脾脏增大、变厚,约占据6个肋单元。
CT诊断:食管裂孔疝、肝硬化伴胃及腹水疝入胸腔。
讨论:食管裂孔疝是由于食管裂空处先天发育不良或某些继发因素,所导致的腹压增高,导致膈食管裂孔部变松弛,腹腔内脏器通过食管裂孔进入胸腔。病理、临床及X线均分为可复性(滑动性)食管裂孔疝及不可复性(包括嵌顿性)食管裂孔疝。症状轻者临床无明显症状,重者常出现上腹饱胀、呃气、返酸和呕吐。可复性疝症状为间歇性,如果症状持续性加重,提示嵌顿性疝的可能。
 图1
图1
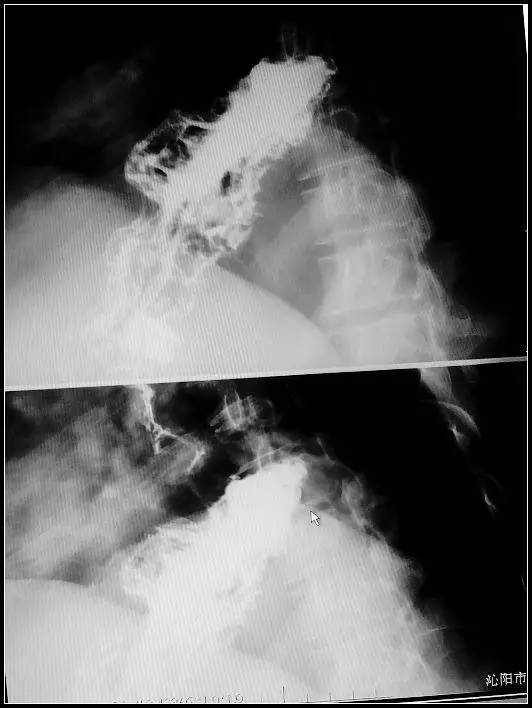 图2
图2
 图3
图3
 图4
图4
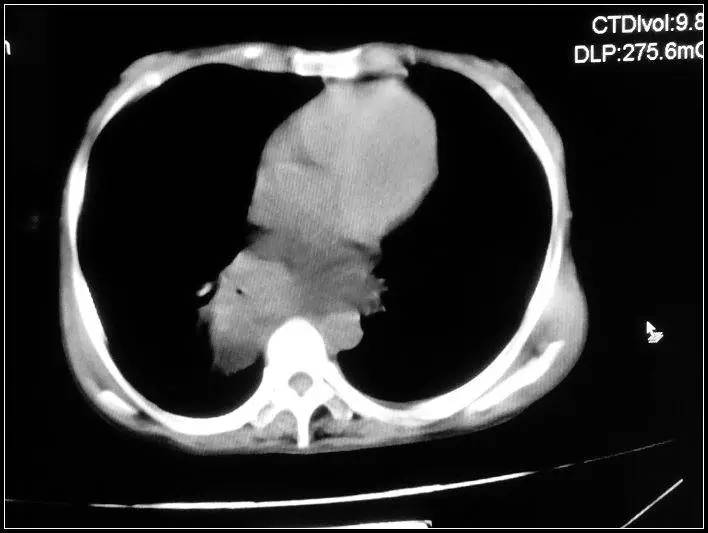 图5
图5
 图6
图6
 图7
图7
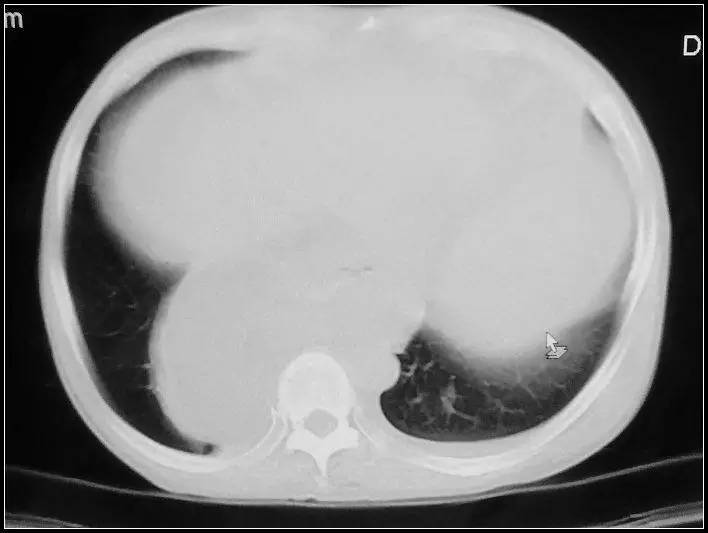 图8
图8
 图9
图9
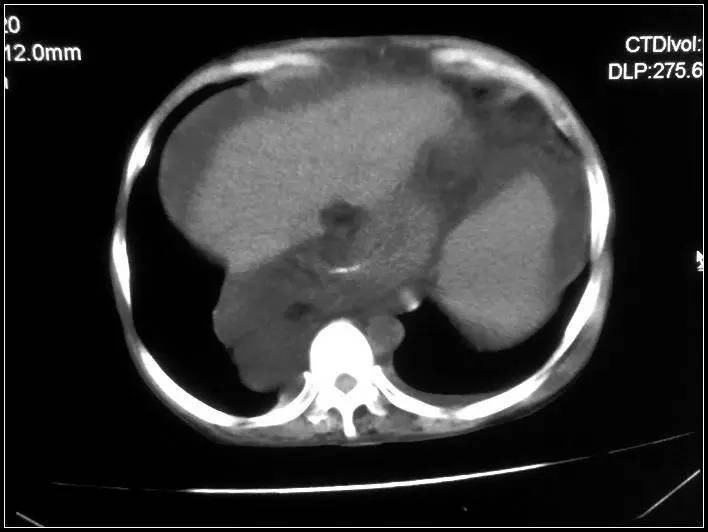 图10
图10
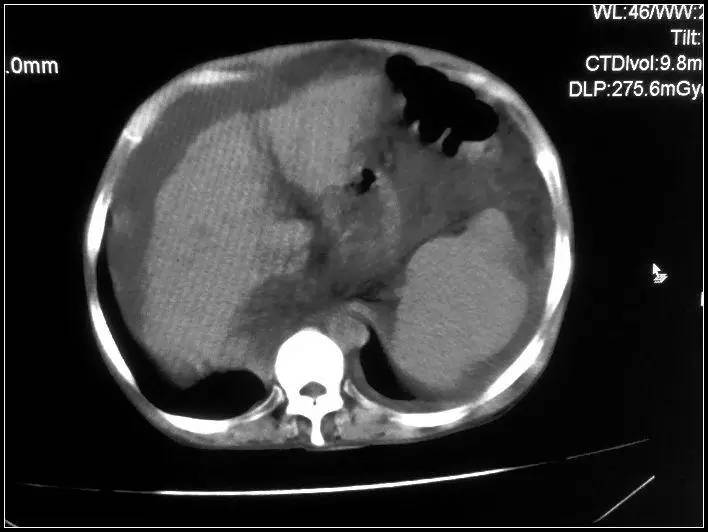 图11
图11
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章,值得分享。
47
#食管裂孔疝#
53
#食管#
39
#疝#
52