PNAS:新发现:抗疟疾药物苯芴醇有望治疗脑肿瘤
2020-05-29 Lauren 转化医学网
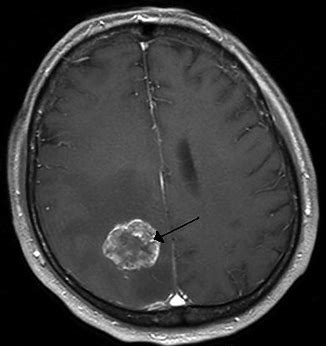
导言:多形性胶质母细胞瘤是胶质瘤(GBM)的一种,是属于恶性程度最高的脑肿瘤之一。胶质瘤是颅内最常见的恶性肿瘤,可以占所有颅内肿瘤的百分之40到50%。目前的治疗标准包含放疗和替莫唑胺,能够在一定程度
导言:多形性胶质母细胞瘤是胶质瘤(GBM)的一种,是属于恶性程度最高的脑肿瘤之一。胶质瘤是颅内最常见的恶性肿瘤,可以占所有颅内肿瘤的百分之40到50%。目前的治疗标准包含放疗和替莫唑胺,能够在一定程度上延长多形性胶质母细胞瘤患者的生命,但GBM对这些治疗的耐受性却屡见不鲜。最近发表在《PANS》杂志上的一项新研究表明,抗疟药物苯芴醇有望治疗脑癌。
多行性成胶质母细胞瘤(GBM)是一种侵袭性脑肿瘤,通常具有致命性。但VCU癌症中心和VCU分子医学研究所的研究人员有了新的发现,通过添加苯芴醇(Imufantrine)(一种FDA批准的用于治疗疟疾的药物)能够增提高当前最常见的脑癌治疗方法的有效性。
目前的治疗标准包含放疗和替莫唑胺(一种抗癌的化疗药物),能够在一定程度上延长多形性胶质母细胞瘤患者的生命,但GBM对这些治疗的耐受性却屡见不鲜。此外,接受标准方法治疗GBM的患者的5年存活率不到6%,且当前没有任何治疗方法可以预防这种肿瘤的复发。
研究人员一直致力于找出FDA批准的药物和更多罕见的药物,这些药物可能潜在地中和成纤维母细胞瘤对治疗的耐药性和有效性。这项研究在5月14日发表在《美国国家科学院院刊》(Proceedings of the National Academy of Sciences)杂志上,该研究的主要调查员、FNAI的博士保尔·费舍尔(Paul B. Fisher)表示,“我们的研究找出了一种抗疟疾药物的新的潜在用途,可以用来治疗多形性成纤维母细胞瘤,多形性成纤维母细胞瘤对化疗和苯芴醇的标准治疗有耐药性。
更具体的说,苯芴醇能够抑制一种参与癌症发展和扩散的基因因子Fli-1,Fli-1能够控制多形性胶质母细胞瘤对化疗和替莫唑胺的耐药性。
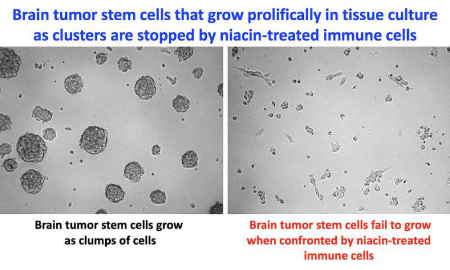
在体外研究(用培养的细胞进行)中,研究人员发现,治疗胶质母细胞瘤时加入苯芴醇可以杀死癌细胞,且抑制肿瘤细胞的生长。这发生在对放疗和替莫唑胺敏感的成纤维细胞瘤和对放疗和替莫唑胺耐药的胶质母细胞瘤中。此外,在体内研究(使用大脑中含有移植的人类多发性胶质母细胞瘤的小鼠进行研究),在治疗敏感和耐药的胶质母细胞瘤细胞中,苯芴醇会抑制肿瘤的生长。
苯芴醇能够中和人体对放疗和化疗的耐受性,基因和分子方法能够识别出新的基因因子“Fli-1”,这是一种重要的能够控制治疗耐药性的基因元素。这一发现成为当前研究的焦点,研究人员找出了“热休克蛋白B1”,也被称为HSPB1,在胶质母细胞瘤中非常突出,其表达受Fli-1调节。针对Fli-1抑制剂的创新筛选策略将苯芴醇鉴定为是一种保护因子,能够与Fli-1结合,使其失活,从而抑制调节多形性胶质母细胞瘤的生长、存活和致癌性(引起肿瘤的能力)的重要基因的表达。
此外,细胞外基质(ECM)重塑和上皮-间充质转化(EMT)是胶质母细胞瘤侵袭和扩散的两个关键过程,是调节胶质母细胞瘤抗放化疗能力的重要因素。这两个过程受Fli-1调控,并被苯芴醇抑制。
为了帮助治疗胶质母细胞瘤,研究人员将进一步探索其他方法来对抗Fli-1诱导的治疗抵抗。
费舍尔表示,“这些临床前研究提供了用苯芴醇抑制Fli-1/HSPB1和苯芴醇的结实依据,这是潜在的胶质母细胞瘤治疗的新方法。从FDA批准的治疗剂和不常见的来源中鉴定出诸如苯芴醇类的药物,将为扩大目前针对多形性胶质母细胞瘤患者的治疗方案的广度和多功能性提供机会。”
研究人员表示,除胶质母细胞瘤外,Fli-1的表达在黑素瘤,卵巢癌,乳腺癌和其他癌症中也可见到,这表明阻断Fli-1的促癌作用也可能对其他癌症患者有所帮助。
费舍尔说:“目前的结果可能比仅仅治疗胶质母细胞瘤具有更广泛的意义。”
原始出处:
Yetirajam Rajesh, Angana Biswas, Utkarsh Kumar, et.al. Lumefantrine, an antimalarial drug, reverses radiation and temozolomide resistance in glioblastoma. PNAS May 14, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新发现#
24
#抗疟疾#
42
#抗疟疾药物#
39
#PNAS#
0
#脑肿瘤#
35