J Am Acad Dermatol:Ustekinumab治疗儿童斑块型银屑病的真实经验
2022-03-06 医路坦克 MedSci原创
对ustekinumab治疗儿童斑块型银屑病的有效性和安全性的了解有限,本实验评估其在儿童和青少年中的真实经验,结果表明Ustekinumab是治疗儿童斑块型银屑病的一种有效、安全的生物制剂。
我们对ustekinumab治疗儿童斑块型银屑病的有效性和安全性的了解仅限于两个3期临床试验,为了评估这种生物制剂在儿童和青少年中的真实经验,我们在加拿大卡尔加里的一个社区皮肤科诊所进行了回顾性图表审查。
23例中重度斑块型银屑病患儿的人口学特征和临床特征如表一所示。初始剂量为:0.75 mg/kg(体重<6 0 kg),45 mg(体重≥60 kg和≤10 0 kg),或90 mg(体重>10 0 kg)皮下注射,0周和4周,然后每12周一次。主要应答者被定义为16周时调查者总体评估(IGA)评分为0或1(IGA 0/1)。次级应答者在52周时IGA为0/1,但在第16周未达到。安全性通过记录治疗开始后的不良事件(AES)进行评估。
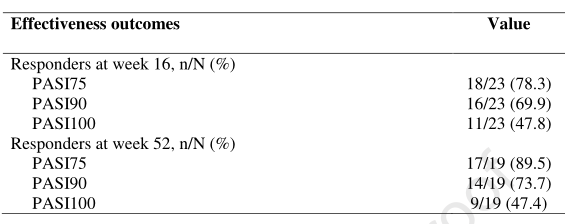
在23名患者中,78.3%为一级应答者,17.4%为二级应答者;一名一级应答者在52周时未维持免疫球蛋白0/1。16周时:银屑病平均面积和严重程度指数从13.3%降至2.4%(p=0.0001;表II),较基线改善75%(PASI75)、90%(PASI90)和100%(PASI100)的患者比例分别为78.3%、69.9%和47.8%;平均体表面积和平均儿童皮肤病生活质量指数分别由14.2%降至1.8%(p=0.0001)和9.4%降至2.7%(p=0.0001)。52周时:平均PASI0.9(p=0.0001);PASI75、PASI90和PASI100分别为89.5%、73.7%和47.4%(表II);平均BSA为0.2%(p=0.0001);平均CDLQI2.0(p=0.0001)。
表一.接受ustekinumab治疗的儿童斑块型银屑病患者的基线人口学和临床特征。缩写:BSA,身体表面积;CDLQI,儿童皮肤病生活质量指数;IGA,研究者全球评估;PASI,牛皮癣面积和严重程度指数。

表二:儿童斑块型牛皮癣患者在接受ustekinumab治疗后第16周和52周的疗效结果。缩写:PASI75,牛皮癣面积和严重指数较基线改善75%;PASI90,牛皮癣面积和严重指数较基线改善90%;PASI100,牛皮癣面积和严重指数较基线改善100%。
69.5%的患者需要剂量优化:13.0%的患者剂量增加(超出体重调整),26.1%的患者间隔减少,30.4%的患者同时要求剂量增加和间隔减少。常见的伴随疗法是外用皮质类固醇/维生素D3类似物(60.9%)、外用皮质类固醇(26.1%)和甲氨蝶呤(21.7%)。尽管剂量优化,4.3%的患者是原发性或继发性无反应者,并改用另一种生物疗法。结果在很大程度上与给药方案、辅助治疗、先前的生物暴露和特殊部位受累无关;只有第52周按辅助治疗分层的平均PASI显示出任何显著差异
没有严重的不良反应或特别感兴趣的不良反应的报道;1名患者出现注射部位反应。没有因急性呼吸综合征而中断治疗,也没有任何实验室检测确认的SARS-CoV-2感染。
我们的发现与之前的临床试验结果是一致的。Landells等人报道称,在接受ustekinumab治疗的患者中,分别有80.6%、61.1%和38.9%的患者在第12周达到PASI75、PASI90和PASI100,应答维持在52周。类似的结果显示,接受ustekinumab治疗的患者中,分别有84.1%、63.6%和34.1%的患者在第12周达到PASI75、PASI90和PASI100,而在52周时反应维持或增加。
我们的研究表明,Ustekinumab是治疗儿童斑块型银屑病的一种有效、安全的生物制剂。这项研究的局限性包括其回溯性和相对较小的样本量。
文献来源:Ladha MA, Rankin BD, Adly M,Real-world experience with ustekinumab for the treatment of plaque psoriasis in pediatric patients: a retrospective, single-center chart review.J Am Acad Dermatol 2022 Feb 19;

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ACA#
43
#ustekinumab#
40
#mAb#
26
#斑块#
39
#斑块型银屑病#
33
认真学习了
47