ESC 2014:无心衰稳定性冠心病患者的心率管理(SIGNIFY 试验)
2014-09-02 cath 编辑 医学论坛网
ESC 2014公布的SIGNIFY研究表明,进一步降低心率至55-60bpm未改善未改善无临床心力衰竭的稳定性冠心病(SCAD)患者预后。相关文章在线发表于《新英格兰医学杂志》(简称NEJM),摘要号为ISRCTN61576291。 SIGNIFY名为评价If抑制剂伊伐布雷定对冠状动脉疾病患者发病率和死亡率益处的随机双盲安慰剂对照研究,入选了51个国家的19102例SCAD患者,基础窦性静息心
ESC 2014公布的SIGNIFY研究表明,进一步降低心率至55-60bpm未改善未改善无临床心力衰竭的稳定性冠心病(SCAD)患者预后。相关文章在线发表于《新英格兰医学杂志》(简称NEJM),摘要号为ISRCTN61576291。
SIGNIFY名为评价If抑制剂伊伐布雷定对冠状动脉疾病患者发病率和死亡率益处的随机双盲安慰剂对照研究,入选了51个国家的19102例SCAD患者,基础窦性静息心率≥70bpm,不伴临床心力衰竭且左室射血分数(LVEF)>40%。研究者们将其随机分为安慰剂组和伊伐布雷定组,剂量调整至目标心率为55-60次/分,主要终点为心血管死亡或非致死性心肌梗死复合终点。
3个月时,伊伐布雷定组和安慰剂组患者平均心率分别为60.7±9.0次/分和70.6±10.1次/分。中位随访27.8个月时,两组主要终点发生率无显著差异(6.8% vs. 6.4%,P=0.20)。
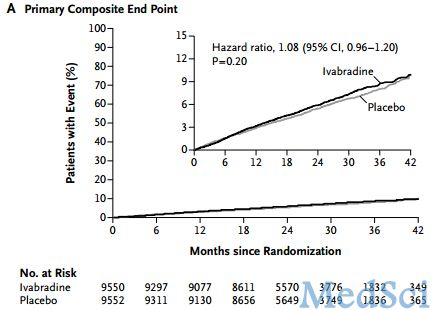
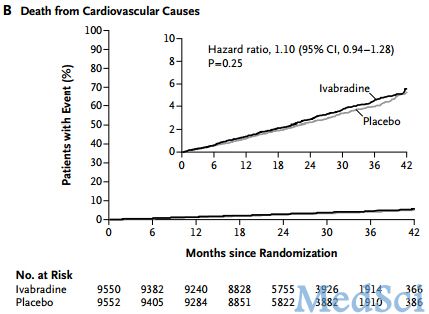
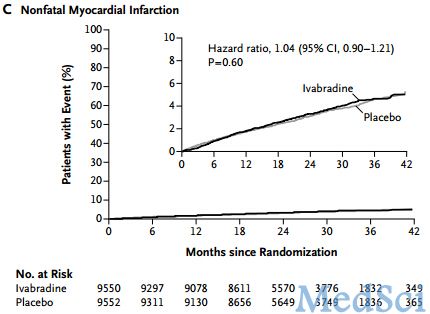
Figure 1. Kaplan–Meier Plots of the Primary Composite End Point and Its Components
在活动受限的心绞痛患者中,伊伐布雷定与终点事件发生率增加相关,而在无活动受限的心绞痛患者中并无上述相关性。
与安慰剂组相比,伊伐布雷定组的心动过缓发生率较高(18.0% vs. 2.3%, P<0.001)。
原始出处:
Kim Fox, M.D., Ian Ford, Ph.D., Philippe Gabriel Steg, M.D., Jean-Claude Tardif, M.D., Michal Tendera, M.D., and Roberto Ferrari, M.D. for the SIGNIFY Investigators.Ivabradine in Stable Coronary Artery Disease without Clinical Heart Failure.NEJM August 31, 2014DOI: 10.1056/NEJMoa1406430[pdf free]

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#稳定性#
25
#心率管理#
30
#Sign#
36
#冠心病患者#
27