J Clin Oncol:纳武单抗联合低剂量伊匹单抗一线治疗MSI-H/dMMR转移性结直肠癌的疗效
2021-10-14 Nebula MedSci原创
纳武单抗联合低剂量伊匹单抗作为一线治疗在MSI-H/dMMR mCRC 患者中展现出了强大且持久的临床效益和良好的耐受性
基于CheckMate 142研究,纳武单抗(Nivolumab)获得了美国FDA批准作为单药或联合伊匹单抗(Ipilimumab)用于治疗微卫星不稳定性高/错配修复缺陷(MSI-H/dMMR)的经氟嘧啶、奥沙利铂和伊立替康治疗后进展的转移性结直肠癌(mCRC)。
本文报告了II期CheckMate 142研究中纳武单抗联合低剂量伊匹单抗作为一线治疗方案用于MSI-H/dMMR CRC患者的结果。
既往未治疗过的转移性MSI-H/dMMR CRC患者接受纳武单抗(1次/2周)联合低剂量伊匹单抗(1次/6周)治疗,直到病情进展。主要终点是客观缓解率。
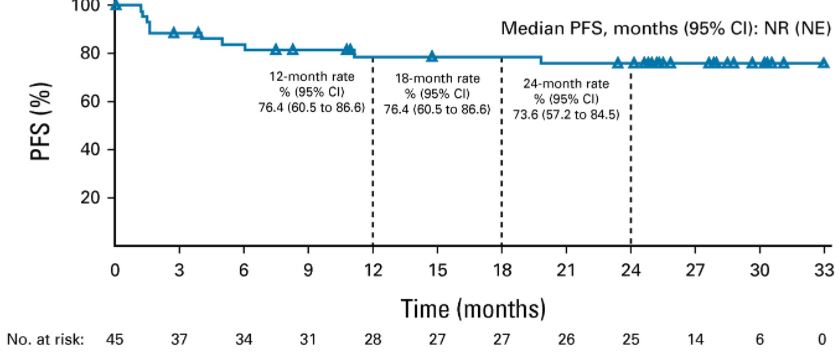
无进展生存率
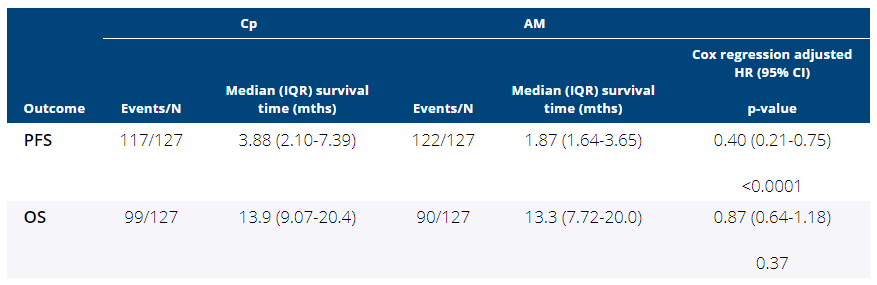
共招募了45位患者,中位年龄为66岁。中位随访了29.0个月。客观缓解率和疾病控制率分别是69%(95% CI 53-82)和84%(95% CI 70.5-93.5),完全缓解率为13%。中位缓解持续时间未达到;74%的缓解患者在截止日期时仍处于缓解状态。
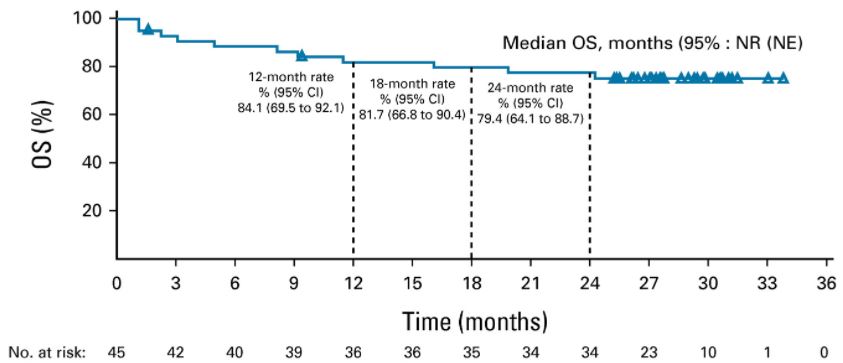
总生存率
最短随访了24.2个月时,中位无进展生存期和中位总生存期均未达到;24个月时的无进展生存率和总生存率分别是74%和79%。无论基线人口统计学和肿瘤特征如何(包括BRAF和KRAS突变状态),均观察到临床获益。在事后分析中,14位未继续治疗也未接受后续治疗的患者中有10位仍未发生进展。在整个研究期间,患者报告的预后保持稳定。
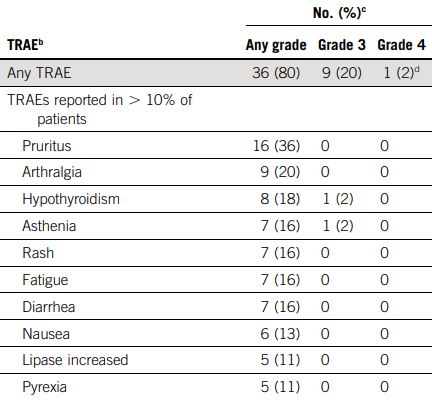
不良事件发生情况
22%的患者发生了3-4级的治疗相关的不良事件;13%的患者因治疗相关不良事件而终止治疗。
综上所述,纳武单抗联合低剂量伊匹单抗作为一线治疗在MSI-H/dMMR mCRC 患者中展现出了强大且持久的临床效益和良好的耐受性。基于这些数据,可进一步开展相关随机试验。
原始出处:
Heinz-Josef Lenz, et al. First-Line Nivolumab Plus Low-Dose Ipilimumab for Microsatellite Instability-High/Mismatch Repair-Deficient Metastatic Colorectal Cancer: The Phase II CheckMate 142 Study. Journal of Clinical Oncology. October 12, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.01015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
42
#转移性#
28
#结直肠#
38
#低剂量#
45
#MMR#
45
#MSI#
31