GUT:中高危胃肠化生患者要定期内镜检查评估肠化生情况,预防胃癌
2021-05-17 MedSci原创 MedSci原创
胃癌(GC)是世界上第五大常见癌症和第三大癌症相关死亡原因,死亡率高的主要原因是发病较晚。超过70%的国家报告了胃癌的高死亡率/发病率(>0.8)。只有日本和韩国的死亡率/发病率较低(分别为0.

胃癌(GC)是世界上第五大常见癌症和第三大癌症相关死亡原因,死亡率高的主要原因是发病较晚。超过70%的国家报告了胃癌的高死亡率/发病率(>0.8)。只有日本和韩国的死亡率/发病率较低(分别为0.43和0.35),这两个国家都有政府资助的内镜检查项目。胃癌筛查的成本效益很大程度上取决于该地区胃癌的发生率和内镜检查的成本。在中或低GC发病率的国家采用全民内镜筛查方法是不划算的。对于这些区域,内镜针对性筛查高危个体可能是更好的方法。因此,风险分层将是指导内镜筛查的一个适当策略。
GC的流行亚型通过一系列可识别的癌前阶段发展—炎症、萎缩、肠上皮化生(IM)、非典型增生和癌。对这些癌前阶段的患者进行监测,可能有助于早期诊断胃癌,从而提高生存率。胃癌前病变在日常实践中很常见,欧洲胃肠内镜协会推荐对胃癌前病变进行内镜监测,然而,胃癌前病变监测的临床采用率仍然很低,主要原因是缺乏来自大型前瞻性研究的支持性临床证据、异质性抽样和报告实践以及实施人群水平筛查的成本。
为了保证胃炎前病变的均匀报告,我们介绍了可操作与胃癌风险相关胃炎评估 (operation Link of Gastritis Assessment, OLGA)。多项研究表明,OLGA可靠地确定了一个具有胃癌高危的亚群(OLGA III-IV期)患者。然而,OLGA是以胃萎缩的组织学参数为基础的,在这一点上,观察者间的一致性较差。另一些人则主张通过可操作性胃癌风险相关的肠化生评估(operation Link on gastric Intestinal Metaplasia, OLGIM)使用IM来代替胃萎缩。与OLGA相比,OLGIM报告了高水平的观察者间一致性,并将较少的患者分类到III和IV高危阶段。需要更多的研究来验证OLGIM并支持其临床应用。
Jonathan W J Lee等开展了一项前瞻性研究,调查IM患者早期胃肿瘤(EGN)的发生率,并验证OLGIM对IM患者风险分层的实用性。发表在GUT杂志。
这是一项前瞻性、纵向和多中心研究。研究参与者包括2980名患者,从2004年1月到2010年12月,他们接受了标准胃粘膜取样的筛选胃镜检查,并在第3年和第5年定期接受内镜检查。参与者还与国家疾病登记办公室进行了早期胃肿瘤漏诊(EGN)比对。有21名参与者被诊断为EGN。IM是EGN的一个重要危险因素(调整后HR 5.36;95% CI 1.51 - 19.0;术中,0.01)。年龄调整后的EGN发病率分别为133.9和12.5 / 10万人-年。OLGIM III-IV期的参与者风险最大(调整后HR 20.7;95% CI 5.04至85.6;术中,0.01)。超过一半(n=4/7)属于基线OLGIM III-IV的egn在2年内出现(范围:12.7-44.8个月)。血清三叶因子3 (Area Under the Receiver Operating Characteristics, 0.749)可区分幽门螺杆菌阴性的OLGIM III-IV患者。OLGIM II患者的EGN风险也显著(调整后的HR为7.34;95% CI 1.60 - 33.7;p = 0.02)。在OLGIM II-IV期患者中,显著的吸烟史进一步增加EGN的风险。
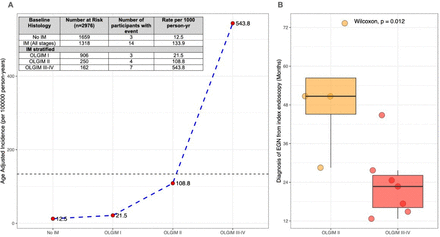
(A)年龄调整后的早期胃肿瘤(EGN)发病率按基线胃肠上皮化生(OLGIM)分期的手术联系分层。(B)框图显示OLGIM II型(橙色)和OLGIM III-IV型(红色)患者发生EGN的时间(年),中位时间(中线)分别为50.7个月(范围28.5-73.3)和22.7个月(范围12.7-44.8)。第25和75分位数由盒子的下端和上端表示。IM,肠上皮化生。

(A)根据阴性状态(HP−;左列)或阳性状态(HP+;右列)的HP血清学跨越基线OLGIM分期(x轴)。血清浓度采用log2单位进行方差转换,统计学差异通过方差分析进行检验。(B)血清生物标志物(TFF3, MIF,胃蛋白酶原I/II比值)与阴性状态(HP−;左列)或阳性状态(HP+;(右列)的HP血清学及其分类定义(OLGIM II-IV vs OLGIM 0-I;或(OLGIM III-IV vs OLGIM 0-II,底行)。
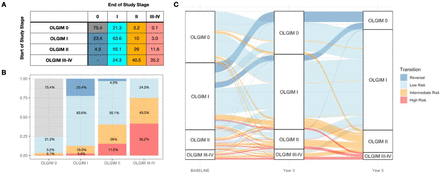
(A) 随后的OLGIM分期(列)在5年分层。每个细胞代表该基线OLGIM期患者与相应研究OLGIM期结束的比例(%)。细胞以颜色表示无IM(灰色)、逆转(蓝色)、低风险(浅蓝色)、中风险(橙色)和高风险(红色)的过渡状态。(B)柱状图,表示每个基线OLGIM阶段患者出现过渡状态的比例(%)(x轴):无IM(灰色)、逆转(蓝色)、低风险(浅蓝色)、中风险(橙色)、高风险(红色)。(C) GCEP患者的冲积流程图:该图仅包括至少一次内镜检查诊断为胃IM的患者。流程图遵循每个患者基线内镜(分层OLGIM阶段)和病人的后续访问3和访问5 OLGIM阶段,即病人轨迹由相应的过渡状态轨迹概括:没有IM(灰色),反转(蓝色),低风险(浅蓝色),中间风险(橙色)和高风险(红色)。
内镜监测目标人群的风险分层可能带来潜在的优势。在中低胃癌发病率的国家,通过OLGIM风险分层优先进行内窥镜监测,可提高胃癌的早期发现、及时的治疗干预和降低胃癌死亡率。
这项研究再次证实IM患者存在EGN风险。然而,EGN的风险在OLGIM II-IV期患者中最为明显,占IM患者的三分之一(31.4%)。伴有晚期OLGIM分期的EGN风险增加重申了IM严重分级和广泛扩散是其肿瘤进展的关键预测指标。之前,只有OLGIM III-IV被报道为内镜监控的高危状态,被推荐在3年内进行内镜监控。这项研究显示OLGIM II期也具有EGN的显著风险,尽管在这些病例中,EGN的进展需要更长的时间(中位数50.7个月;范围28.5 ~ 73.3个月),而OLGIM III ~ IV期病变(中位22.7个月;范围12.7 - -44.8个月)。因此,研究结果提示,OLGIM III-IV期患者可在早期2年重复内镜检查中获益,OLGIM II期患者可在4-5年重复内镜检查中获益。采用绝对风险降低分析,OLGIM I、II、III-IV期患者中,通过每年两次常规内镜监测检测到一种EGN的最少人数分别为485、60和18。
综上所述,GCEP研究队列设于GC低、中发病率人群,显示IM患者发生EGN的风险增加。然而,大多数IM患者具有低风险的IM表型,5年内可能没有肿瘤进展。然而,对于一部分高危和中危IM患者,及时的内镜检查者未见到晚期GC。OLGIM风险分层为高危患者(OLGIM III-IV)在2年内进行早期内镜检查和中危患者(OLGIM II)在5年内进行内镜检查提供了一种可行的方法。而绝大多数没有化生或局灶性IM (OLGIM 0-I)的患者可能不需要内镜监视。该研究团队希望临床能够提高风险意识,鼓励临床采用标准化的胃粘膜取样和OLGIM组织学报告。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习学习
58
#内镜#
29
#肠化生#
37
赚积分
58
太棒了
52