Lancet Neurol:郑州大学薛孟周教授综述脑出血后炎症相关继发性损伤与保护机制
2020-12-31 Bio生物世界 Bio生物世界
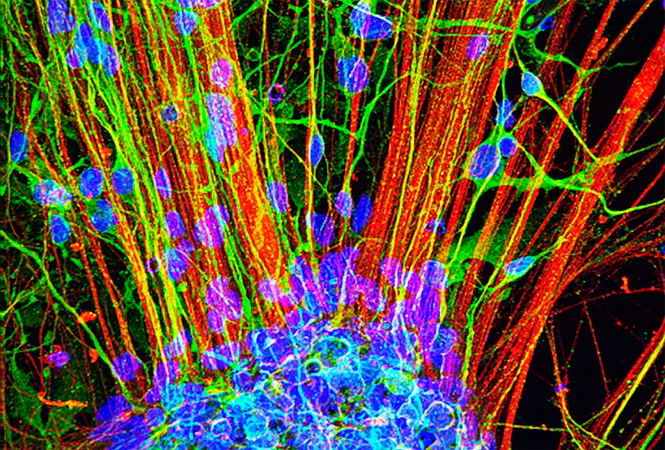
尽管经历了数十年科学研究与医疗技术的进步,脑出血患者的预后仍不尽人意,亟需更为有效的干预措施。脑出血发生后脑内炎症级联反应与其介导的继发性脑损伤可能是预后不良和治疗的关键靶点。
近日,郑州大学脑血管病科主任、河南省脑血管病转化医学重点实验室主任薛孟周教授团队在神经病学领域国际顶级期刊 The Lancet Neurology(影响因子为30.039)发表了题为:Neuroinflammation in intracerebral haemorrhage: immunotherapies with potential for translation 的论文。
这是薛孟周团队今年在Brain(影响因子为11.814)发表 Microglia and macrophage phenotypes in intracerebral haemorrhage injury: therapeutic opportunities 论文后的又一力作。
尽管经历了数十年科学研究与医疗技术的进步,脑出血患者的预后仍不尽人意,亟需更为有效的干预措施。脑出血发生后脑内炎症级联反应与其介导的继发性脑损伤可能是预后不良和治疗的关键靶点。
薛孟周教授团队发表的该篇论文详尽而扼要地综述了脑出血后炎症相关继发性损伤与保护机制,总结并阐释了最具转化潜力的脑出血免疫治疗药物,为该领域基础和临床研究的进一步发展提供了宝贵的指导与借鉴。
The Lancet Neurology 杂志创刊于2002年5月,在临床神经病学领域期刊中排名第一。该杂志以发表权威、独立、最高质量的神经病学研究论文为宗旨,被全世界神经科医师与神经病学研究者奉为标尺。
薛孟周,医学博士,国务院政府特殊津贴专家,郑州大学学科特聘教授,博士生导师,河南省脑血管病重点学科主任,河南省神经病学特聘学科带头人,河南省脑血管病转化医学创新型科技团队带头人,郑州大学第二附属医院脑血管病学主任。发表SCI论文70余篇,总影响因子超过360分,总引用次数超过3000次,会议论文160余篇。
薛孟周教授一直致力于脑出血的相关研究,曾在国际上报道了自体血注射的脑出血动物模型,被学界认可并广泛引用达900余次。
原始出处:
Mengzhou Xue, V Wee Yong.Neuroinflammation in intracerebral haemorrhage: immunotherapies with potential for translation . Lancet Neurol . 2020 Dec;19(12):1023-1032. doi: 10.1016/S1474-4422(20)30364-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#继发#
39
#继发性#
52
#Lancet#
33
#Neurol#
28
#损伤#
24
顶刊就是不一样,质量很高,内容精彩!学到很多
49
机制研究离临床仍然有距离,不过与临床结合思考,仍然有帮助的,不能仅仅是纯临床思维,转化思维同样重要
54