Small:具有肿瘤细胞内双重荧光增强特性的诊疗探针
2017-05-29 佚名 MaterialsViews
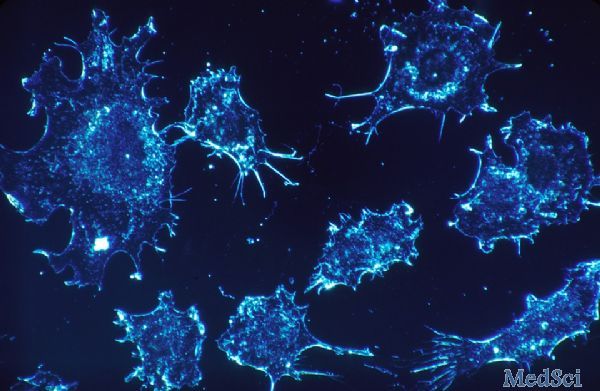
近年来,恶性肿瘤的诊疗一体化已成为材料学和生物医学的热点领域,这为肿瘤的精准治疗开辟了新途径,具有重要的研究意义和临床应用前景。在诊疗一体化制剂的开发中,作为生物探针的荧光材料越来越受到人们的重视,但传统荧光分子极易光漂白、具有聚集诱淬灭现象,且信噪比较低,这大大限制了其在生物医学上的应用。为了克服这一问题,浙江大学计剑教授研究团队开发了一种肿瘤细胞内特异性双重荧光增强的生物探针。与传统荧光标记方
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#探针#
31
#荧光#
35
#肿瘤细胞#
28
#ALL#
30
#SMA#
28
谢谢分享谢谢分享
0
学习了,谢谢分享
65