营养不良小case?可使急性心梗PCI术后死亡风险升高6倍!
2022-01-13 LILYMED MedSci原创
BMC Cardiovascular Disorders:营养状况对经皮冠状动脉介入治疗急性心肌梗死患者预后的影响
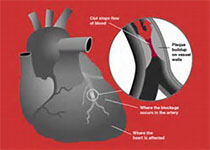
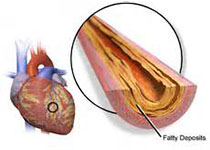
急性心肌梗死(AMI)是全球死亡的主因,在做出医疗决定时,评估AMI患者的死亡风险至关重要。全球急性冠状动脉事件登记处(GRACE)风险评分有助于通过考虑8个因素来估计院内死亡率:年龄、心率、收缩压、初始血清肌酐水平、Killip分类、入院时心脏骤停状态、心脏标志物水平升高和ST段偏差。欧洲心脏病学会和日本循环学会的指南都建议使用该风险评分来估计AMI患者死亡率。

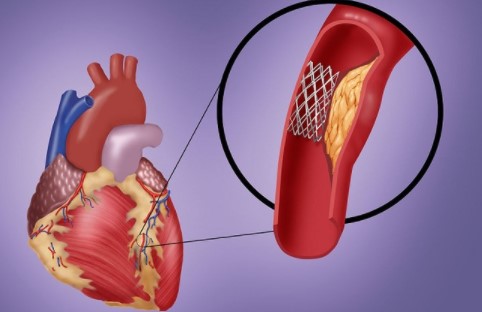
越来愈多证据证明,虚弱和肌肉减少症被认为是影响心血管疾病预后的重要因素。老年营养风险指数(GNRI)被广泛用作使用体重指数(BMI)和血清白蛋白筛查营养状况的简单方法。最近的研究表明,低GNRI与心力衰竭患者的预后恶化及与危重肢体缺血患者的死亡率有关。然而,营养不良与AMI患者死亡率之间的关系尚不清楚。本研究旨在调查GNRI评估的营养不良对AMI患者首次经皮冠状动脉介入治疗(PCI)后死亡率的影响。
1、基线特征
你研究在连续268例接受经皮冠状动脉介入治疗(PCI)的AMI患者中,评估了全因死亡与基线特征(包括营养不良(GNRI <92.0)和全球急性冠状动脉事件登记处(GRACE)风险评分)之间的关联。
表1显示患者的基线临床特征。51例患者(19%)营养不良(GNRI<92.0),而217例患者(81%)没有。比起非营养不良患者(中位数,67岁;IQR,57-75岁),营养不良患者年龄较大(71岁;IQR,66-83岁);p < 0.001)。营养不良组的eGFR和LVEF均低于非营养不良组(p <各0.001)。此外,营养不良组的GRACE风险评分(中位数,166;IQR,132-188)比非营养不良组(中位数,124;IQR, 104–148;p < 0.001)显着更高。

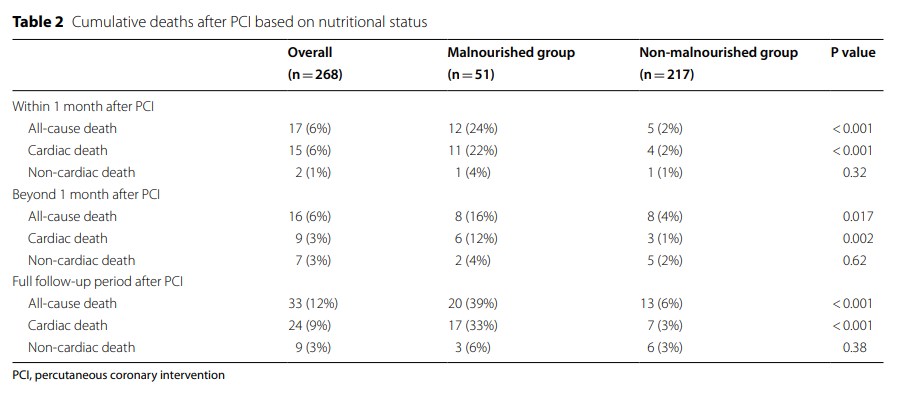
2、营养不良和非营养不良群体 PCI 后的死亡率
随访的中位时间为698天(IQR,503-957天),最大随访时间为1819天。33例患者(12%)在PCI后死亡(表2),其中有24例心脏死亡(心力衰竭,n = 17;心脏破裂,n = 4;心室颤动,n = 3)和9例非心脏死亡(脑梗死,n = 2;败血症,n = 3;癌症,n = 4)。在PCI术后1个月内(各p<0.001)、PCI术后1个月以上(p=0.017和p=0.002)以及PCI术后整个随访期间(各p<0.001),营养不良组的全因和心脏死亡发生率均显著高于非营养不良组(表2)。Kaplan-Meier分析显示,营养不良组的存活率明显低于非营养不良组(p <0.001)(图1)。

3、基线特征对PCI后全因死亡的影响
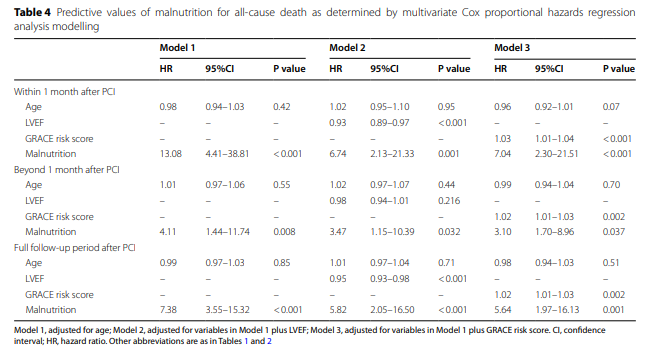
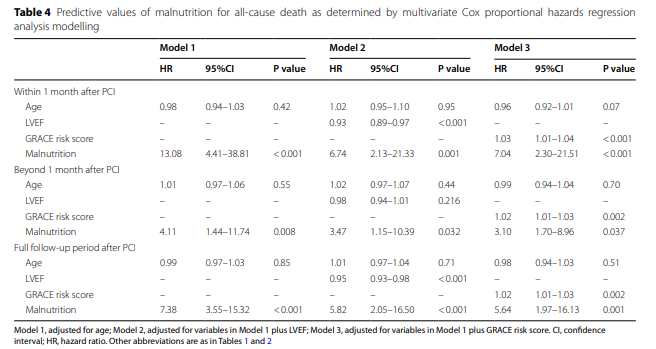
单变量Cox比例风险回归分析显示,GRACE风险评分和营养不良均与PCI术后1个月内(p<0.001和p=0.001)、PCI术后1个月以上(p<0.001和p=0.003)、PCI后全随访期(p<0.001和<0.001)的全因死亡呈正相关。 LVEF与PCI后1个月内(p=0.025)和全随访期(p<0.001)的全因死亡呈负相关(表3)。多变量cox比例风险回归模型显示,营养不良与PCI后1个月内(模型3,HR:7.04,95%CI:2.30–21.51,p <0.001),PCI术后1个月以上(模型3,HR:3.10,95%CI:1.70–8.96,p = 0.037),PCI后全随访期模型3, HR: 5.64, 95%CI: 1.97–16.13, p = 0.001)的全因死亡之间存在很强的关联,即使调整了相关因素(表4)。
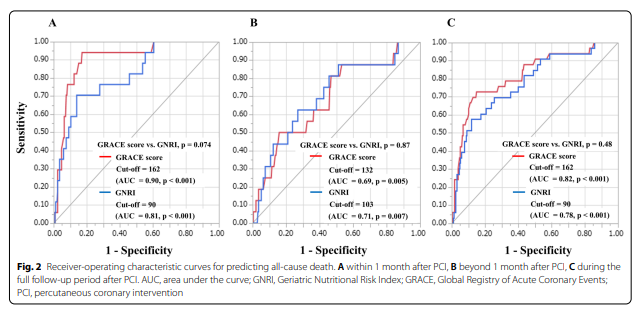
4、GRACE 风险评分和 GNRI 死亡率的预测值
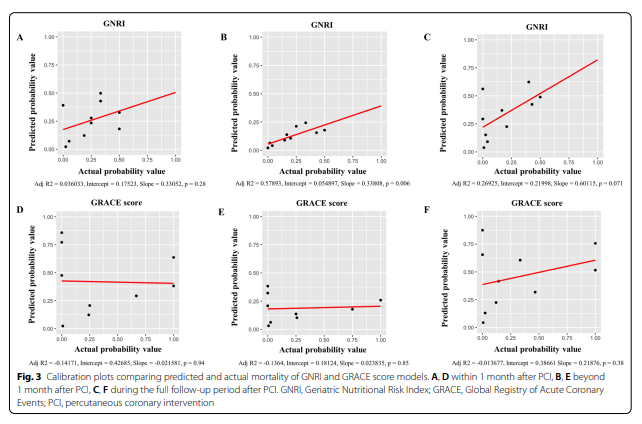
这些结果表明,根据GNRI的评估,营养不良为PCI后全因死亡提供了有效的独立危险因素。在本研究中,GRACE风险评分也与PCI后的全因死亡有关(表4)。因此,我们分析了ROC曲线,以评估GRACE风险评分和GNRI在预测PCI后全因死亡方面的鉴别能力(图2)。全因死亡中GRACE风险评分和GNRI的ROC临界值在PCI后1个月内分别为162和90(AUC = 0.90,p <0.001,AUC = 0.81,p <0.001)(图2A)、 PCI 后 超过1 个月的分别为132 和 103(AUC = 0.69,p = 0.005 和 AUC = 0.71,p = 0.007)(图2B),以及 PCI 后完整随访期间的 162 和 90(AUC = 0.82,p < 0.001 和 AUC = 0.78,p < 0.001)(图2C)无论随访期如何,GRACE风险评分的ROC曲线与预测PCI后全因死亡的GNRI曲线的比较显示,GRACE风险评分和GNRI之间的AUC无显著差异(图2)。Hosmer和Lemeshow测试分析了GRACE风险评分和GNRI预测PCI后全因死亡的LOGISTIC分析的拟合性(GRACE评分;1个月内:p = 0.71,超过1个月:p = 0.31,完整随访期:p = 0.38和GNRI;1个月内:p = 0.43,超过1个月:p = 0.50, 完整的随访周期:p = 0.45)。此外,比较实际和预测死亡率的校准图如图3所示。而GNRI仅在PCI后超过1个月才具有显着相关性。此外,还对营养不良和GRACE风险评分的相互作用进行了测试。结果,营养不良与GRACE风险评分交互作用在PCI术后1个月、PCI术后1个月以上、PCI术后全随访期的p值比较分别为p=0.62、p=0.64、p=0.38。
本研究的主要发现如下:(1)在接受PCI的AMI患者中,营养不良为PCI后1个月内,PCI后1个月以上以及在整个随访期间的全因死亡提供了独立的危险因素;(2)除了GRACE风险评分外,GNRI的营养评估可能单独预测AMI患者的死亡率,特别是长期死亡率。
总的来说,GNRI 可能具有预测 AMI 患者死亡率的潜力,尤其是在 PCI 后 1 个月以上,这与 GRACE 风险评分不同。营养状况评估可能有助于对 AMI 死亡风险进行分层。
原文来源:
Kanda et al. Impact of nutritional status on prognosis in acute myocardial infarction patients undergoing percutaneous coronary intervention.BMC Cardiovascular Disorders (2022) 22:3
https://doi.org/10.1186/s12872-021-02448-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#case#
53
小康社会下,营养不良的不多了吧哈哈
38
#PCI术#
44
说得好
74
#死亡风险#
37
#急性心梗#
62
#PCI术后#
49
#Cas#
29
学习
60
学习
67