J Clin Oncol:派姆单抗治疗不稳定性高的晚期子宫内膜癌的疗效
2022-01-28 Nebula MedSci原创
派姆单抗在既往接受过治疗的晚期 MSI-H/dMMR 子宫内膜癌患者中显示出了强大而持久的抗肿瘤活性,并显示出令人鼓舞的生存预后,而且毒性可控。
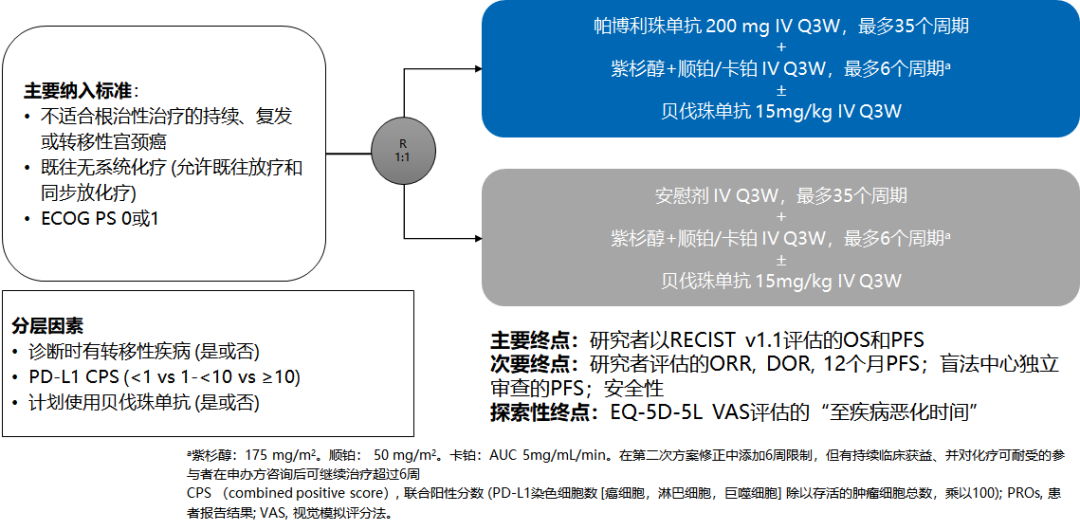
一项 II 期的非随机、开放标签、多队列的临床试验(KEYNOTE-158 研究)中,派姆单抗在既往治疗过的晚期微卫星不稳定性高或错配修复缺陷 (MSI-H/dMMR) 肿瘤(包括子宫内膜癌)患者中表现出持久的抗肿瘤活性。本文报告了 KEYNOTE-158 研究中 MSI-H/dMMR 子宫内膜癌患者的疗效和安全性结果。
D 队列(子宫内膜癌,无论 MSI-H/dMMR 状态如何)和 K 队列(任何 MSI-H/dMMR 的实体瘤,除了结直肠癌)中符合要求的患者,即既往接受过治疗的晚期 MSI-H/dMMR 子宫内膜癌患者,接受派姆单抗 200 mg(1次/周)治疗 35 疗程。主要终点是客观缓解率。次要终点包括缓解持续时间、无进展生存期、总生存期和安全性。
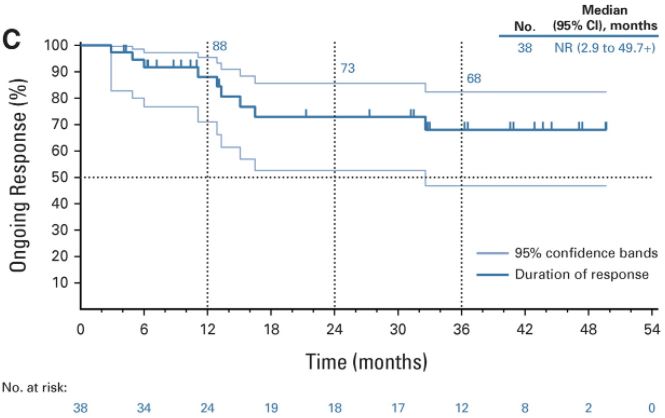
受试患者的缓解率
截止 2020年10月5日,90 位患者中有 18 位(20%)患者完成了 35 疗程的派姆单抗治疗,52 位(58%)患者中断治疗。在疗效评估患者人群(至少接受了一剂派姆单抗和随访≥26周;n=79),从第一剂到截止日期的中位时间是 42.6 个月(范围 6.4-56.1)。
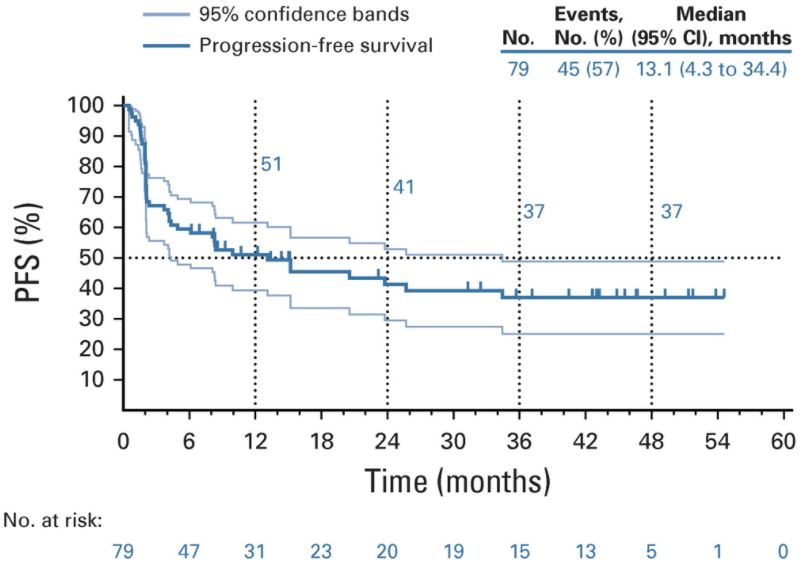
无进展生存期
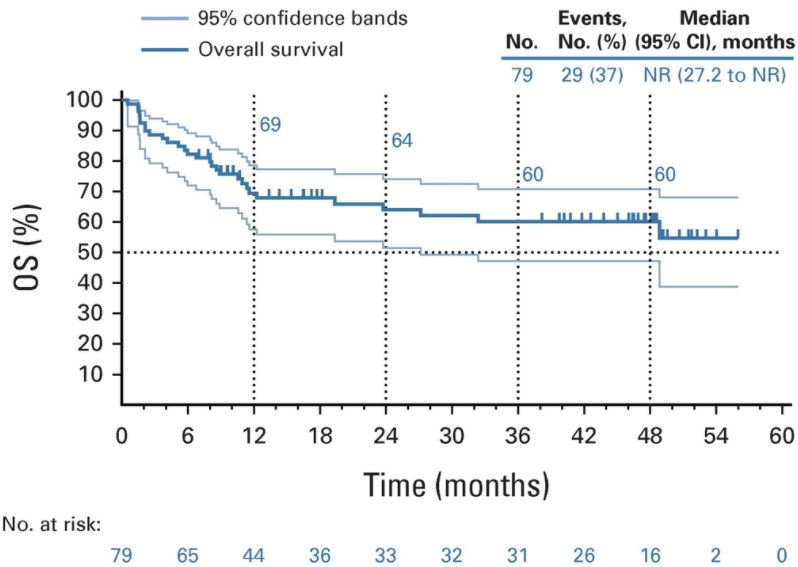
客观缓解率为 48%(95% CI 37-60),中位缓解持续时间未达到(2.9-49.7+个月)。中位无进展生存期为 13.1 个月(95% CI 4.3-34.4),中位总生存期未达到(95% CI 27.2个月-未达到)。
总生存期
在所有接受治疗的患者中,76%的患者至少经历了一次治疗相关的不良反应(3-4级,12%)。无致死性治疗相关事件。28%的患者发生了免疫介导的副反应或输液反应(3-4级,7%,无致死性事件)。
总之,派姆单抗在既往接受过治疗的晚期 MSI-H/dMMR 子宫内膜癌患者中显示出了强大而持久的抗肿瘤活性,并显示出令人鼓舞的生存预后,而且毒性可控。
原始出处:
David M. O'Malley, et al. Pembrolizumab in Patients With Microsatellite Instability–High Advanced Endometrial Cancer: Results From the KEYNOTE-158 Study. Journal of Clinical Oncology. January 06, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.01874
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
34
#内膜#
41
#晚期子宫内膜癌#
43
#子宫内膜癌#
64
#稳定性#
34
#派姆单抗#
52