J Thorac Oncol: 国产PD-1抑制剂信迪利单抗新辅助治疗非小细胞肺癌(NSCLC)的三年随访生存结果
2022-05-23 yd2015 网络 发表于威斯康星
本研究首次报道了PD-1抑制剂作为新辅助治疗的NSCLC患者的长期生存结果。3年的随访显示PD-L1表达阳性、高肿瘤突变负荷患者具有良好的临床疗效。
近期,Journal of Thoracic Oncology杂志上发表了一项临床研究结果,主要是评估国产PD-1抑制剂信迪利单抗新辅助治疗非小细胞肺癌(NSCLC)的三年随访生存结果。

研究的主要终点是AEs、非手术延迟率和手术并发症。关键次要终点为3年总生存率(OS)、1年、2年、3年无病生存率(DFS)、1年、2年、3年无事件生存率(EFS)和主要病理应答(MPR)。
从2018年3月6日-2019年3月8日,我们筛选了43例NSCLC患者,最终纳入了40例患者。在40例入组患者中,3 ( 2例(80%)有吸烟史;鳞状细胞癌33例(82.5%);8例(20%)患者为IA期和IB期,14例(30%)患者为IIA期和IIB期,10例( 25%)患者为IIIA期,8例( 20%)患者为IIIB期( 根据TNM第8版肺癌分期);可检测PD-L1表达水平有32例(80%),其中PD-L1表达阳性22例(55%);淋巴结受累25例(62.5%);37例(92.5%)患者在接受新辅助治疗后接受手术,其中R0切除36例,R2切除(纵隔淋巴结侵犯)1例。
不良事件(AEs)和新辅助治疗相关的AEs (TRAEs)分别在32例和21例患者中观察到。
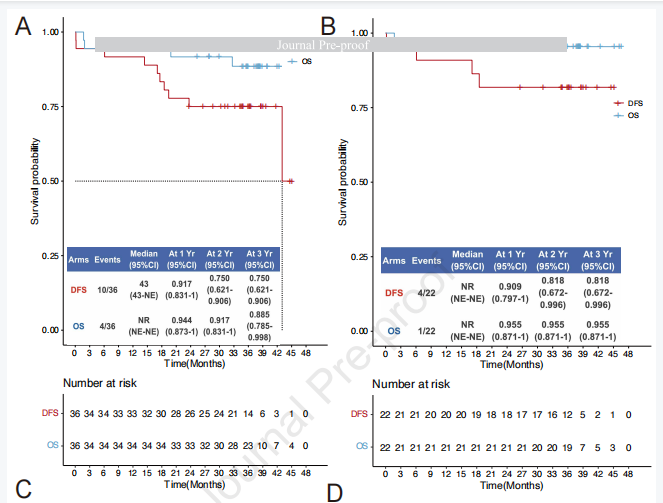
平均随访时间37.8个月(1.73 ~ 46.5个月)。研究分析了两组患者的OS、DFS和EFS:所有患者和PD-L1表达阳性患者(TPS≥1%)。至于OS和DFS,研究纳入了36例R0切除的患者进行分析。随访3年,共有4例患者死亡,6例复发。在36例患者队列中,3年OS为88.5% (95% CI: 78.5-99.8), 3年DFS为75.0% (95% CI: 62.1-90.6)。在PD-L1阳性队列中,随访3年,1例患者死亡,3例复发。在22例PD-L1阳性患者队列中,3年OS率为95.5% (95% CI: 87.1-100), 3年DFS率为81.8% (95% CI: 67.2-99.6)。40例患者被纳入所有患者队列进行EFS评估。中位EFS为44.4个月,3年EFS率为70.0% (95% CI: 57.1-85.7)。在PD-L1阳性队列中,3年的EFS率为81.8% (95% CI: 67.2-99.6)。

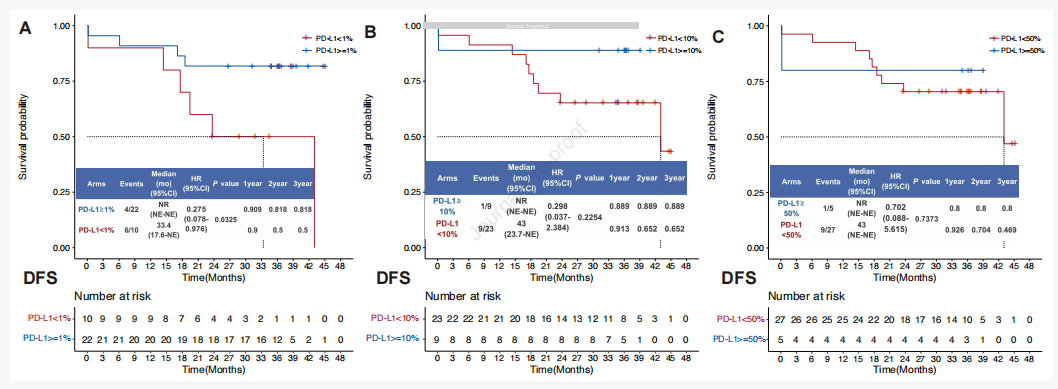
基于DFS和EFS的分析表明PD-L1 ≥1%患者的生存优于PD-L1 <1% (HR, 0.275 [95% CI, 0.078 ~ 0.976];log-rank P = 0.0325)。基于DFS和EFS的分析在分界值为10%和50%的两个亚组之间没有显著性差异,但我们可以观察到与1%分界值相似的趋势(PD-L1 = 10%, HR, 0.298 [95% CI, 0.037 ~ 2.384];log-rank P = 0.2254;PD-L1 = 50%, HR, 0.702 [95% CI, 0.088至5.615];log-rank P = 0.7373)。
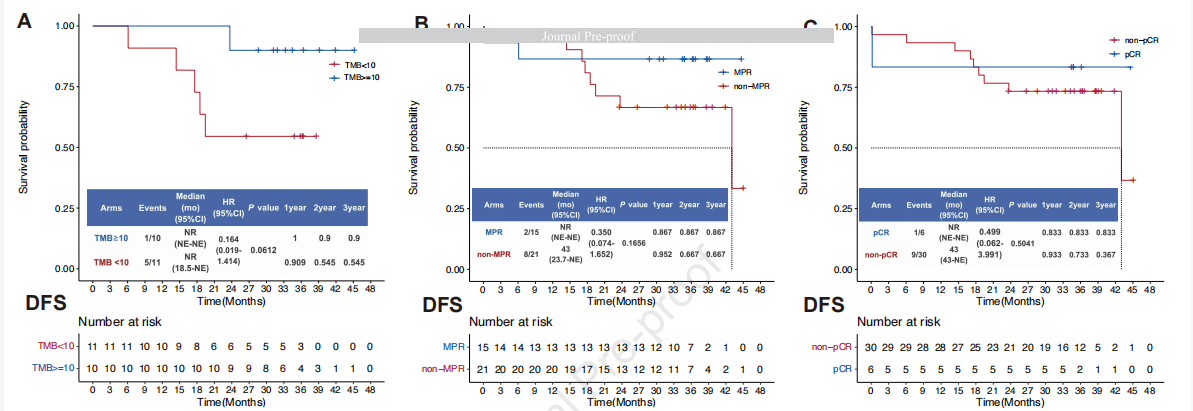
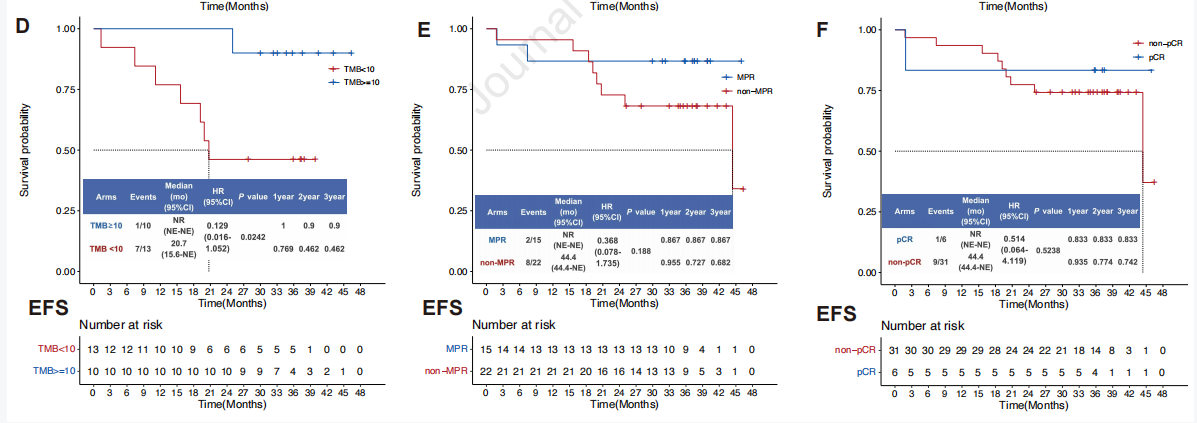
根据DFS和EFS的分析,我们的结果表明,高TMB的患者比低TMB的患者具有更好的临床结局(DFS, HR, 0.164 [95% CI, 0.019 ~ 1.414];log-rank P = 0.0612;EFS, HR, 0.129 [95% CI, 0.016 ~ 1.052];log-rank P = 0.0242)。MPR亚组和pCR亚组在DFS和EFS中无明显差异。然而,MPR组在DFS和EFS方面的3年生存率高于其他亚组(DFS, HR, 0.350 [95% CI, 0.074 ~ 1.652];log-rank P = 0.1656;EFS, HR, 0.368 [95% CI, 0.078 ~ 1.735];log-rank P = 0.1880)。pCR亚组的DFS和EFS的变化趋势相似(DFS, HR, 0.499 [95% CI, 0.062 ~ 3.991];log-rank P = 0.5041;EFS, HR, 0.514 [95% CI, 0.064 ~ 4.119];log-rank P = 0.5238)。
综上,本研究首次报道了PD-1抑制剂作为新辅助治疗的NSCLC患者的长期生存结果。3年的随访显示PD-L1表达阳性、高肿瘤突变负荷患者具有良好的临床疗效。
原始出处:
Zhang F, Guo W, Zhou B, Wang S, Li N, Qiu B, Lv F, Zhao L, Li J, Shao K, Xue Q, Gao S, He J. Research article: Three-year Follow-up of Neoadjuvant PD-1 inhibitor (Sintilimab) in Non-Small Cell Lung Cancer. J Thorac Oncol. 2022 May 9:S1556-0864(22)00216-7. doi: 10.1016/j.jtho.2022.04.012. Epub ahead of print. PMID: 35550174.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#非小细胞#
47
#Oncol#
32
#THORAC#
37
#新辅助#
40
#抑制剂#
39
#PD-1抑制剂#
35
JTO上文章都很好,谢谢梅斯及时上新
38