JAMA Cardiol:高密度脂蛋白胆固醇水平过高,冠状动脉疾病患者死亡风险增加
2022-05-22 MedSci原创 MedSci原创
非常高的HDL-C水平与冠状动脉疾病患者较高的死亡风险相关
既往研究表明,高密度脂蛋白胆固醇 (HDL-C) 水平越高,心血管风险越低。但是,最近在一般人群中的数据显示,在非常高的HDL-C浓度下,不良后果的风险将增加。
该研究旨在探究非常高的HDL-C水平(>80 mg/dL)与冠状动脉疾病(CAD)患者死亡率的相关性,同时评估已知HDL-C基因型与高HDL-C水平结局的相关性。
这是一项前瞻性、多中心的队列研究,从英国生物库(UKB)和埃默里心血管生物库(EmCAB)招募了明确诊断的CAD患者。高HDL-C水平定义:>80 mg/dL。主要终点是全因死亡。次要终点是心血管死亡。
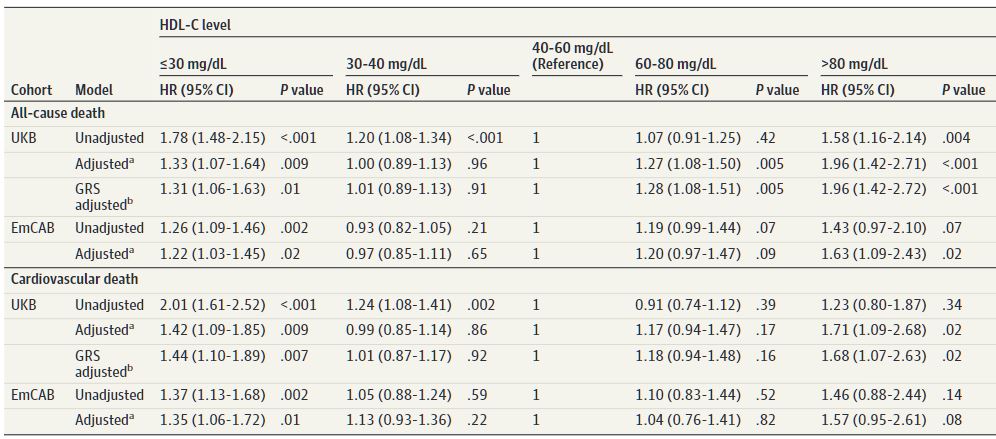
HDL-C水平与不良预后的相关性
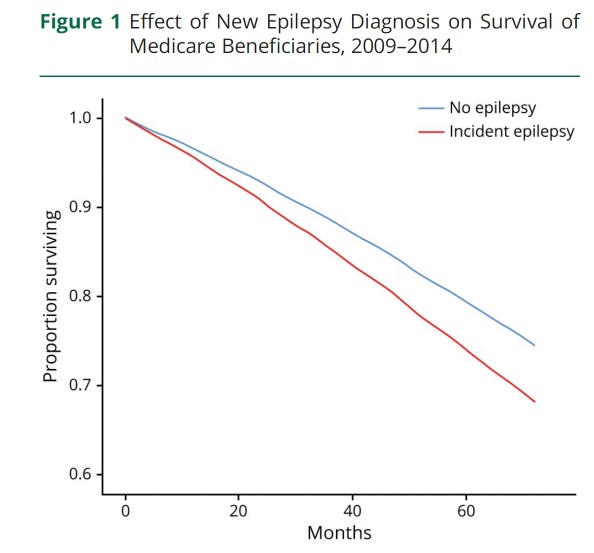
共纳入了14478位受试者(平均62.1岁)。来自UKB和EmCAB的受试者(分别是11034位和5467位)分别中位随访了8.9年和6.7年,与具有中等水平HDL-C的人相比,在低和非常高HDL-C水平的人具有更高的不良临床结局风险,呈“U”形关联。在UKB受试者中,根据混杂因素校正后,与HDL-C水平在40-60mg/dL的人群相比,非常高的HDL-C水平与全因死亡风险(HR 1.96,p<0.001)和心血管死亡风险(HR 1.71, p=0.02)升高相关。该结果在EmCAB受试人群中可重复。
在UKB受试人群中,根据HDL-C遗传风险评分进行调整后,这些关联仍然存在。敏感性分析显示,在UKB受试者中,高HDL-C组男性的全因死亡风险明显高于女性(HR 2.63 [p<0.001] vs 1.39 [p=0.23])。
综上,该研究显示,非常高的HDL-C水平与冠状动脉疾病患者较高的死亡风险相关,而且该关联独立于与高HDL-C水平相关的常见多态性。
原始出处:
Liu C, Dhindsa D, Almuwaqqat Z, et al. Association Between High-Density Lipoprotein Cholesterol Levels and Adverse Cardiovascular Outcomes in High-risk Populations. JAMA Cardiol. Published online May 18, 2022. doi:10.1001/jamacardio.2022.0912
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cardiol#
42
#疾病患者#
56
#患者死亡#
45
#冠状动脉疾病#
38
#死亡风险#
36
#脂蛋白#
57
#高密度脂蛋白胆固醇#
38
JAMA上文章都是顶级的,谢谢梅斯及时上新
37