Nat Commun:急性缺血性卒中后的结果与性别有关
2021-06-03 haibei MedSci原创
最近,研究人员得出了解剖学上的中风病变的低维表征,并设计了一个贝叶斯层次模型框架,专门用于估计与急性中风严重程度有关的病变模式的可能性别差异。
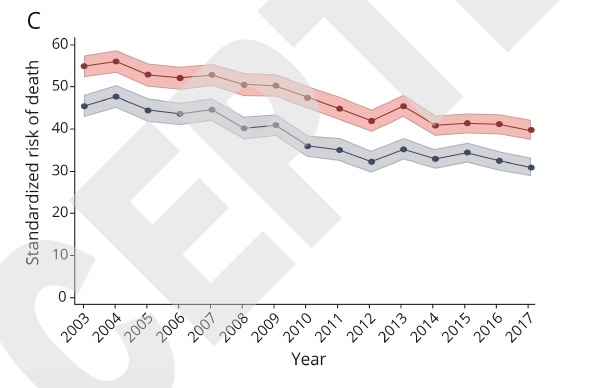
统计数据显示,每年有超过1500万人受到脑卒中的影响。众所周知,它对男性和女性都造成了相当程度的长期损伤。然而,许多流行病学研究表明,在缺血性脑血管疾病的特征中存在与临床相关的性别差异性。例如,由于预期寿命较长,每年发生中风的女性多于男性。预期的人口变化,即人口老龄化,将进一步扩大这一差距:在美国,预测表明,到2030年,将有约20万名女性在中风后致残,而不是男性。
更多的性别差异涉及到女性更经常出现非经典的卒中症状,如疲劳或精神状态的改变,并且有更高的延迟入院的风险。此外,女性因心房颤动而发生心肌栓塞性卒中的风险较高,这可能是女性患者急性缺血性卒中(AIS)严重程度较高的原因。
即使在调整了发病时的年龄、合并症和卒中前的独立程度后,女性卒中严重程度的超标现象仍然存在。重要的是,尽管男性和女性的病灶大小相当,但女性似乎经历了更严重的卒中。事实上,在失语症的案例中也注意到了类似的性别特异性病变体积的影响,即女性引起失语症的病变体积阈值比男性要小。

最近,研究人员得出了解剖学上的中风病变的低维表征,并设计了一个贝叶斯层次模型框架,专门用于估计与急性中风严重程度(美国国家卫生研究院中风量表)有关的病变模式的可能性别差异。该框架是在555名患者(38%为女性)中开发的。研究结果在一个独立的队列中得到了验证(n = 503,41%为女性)。
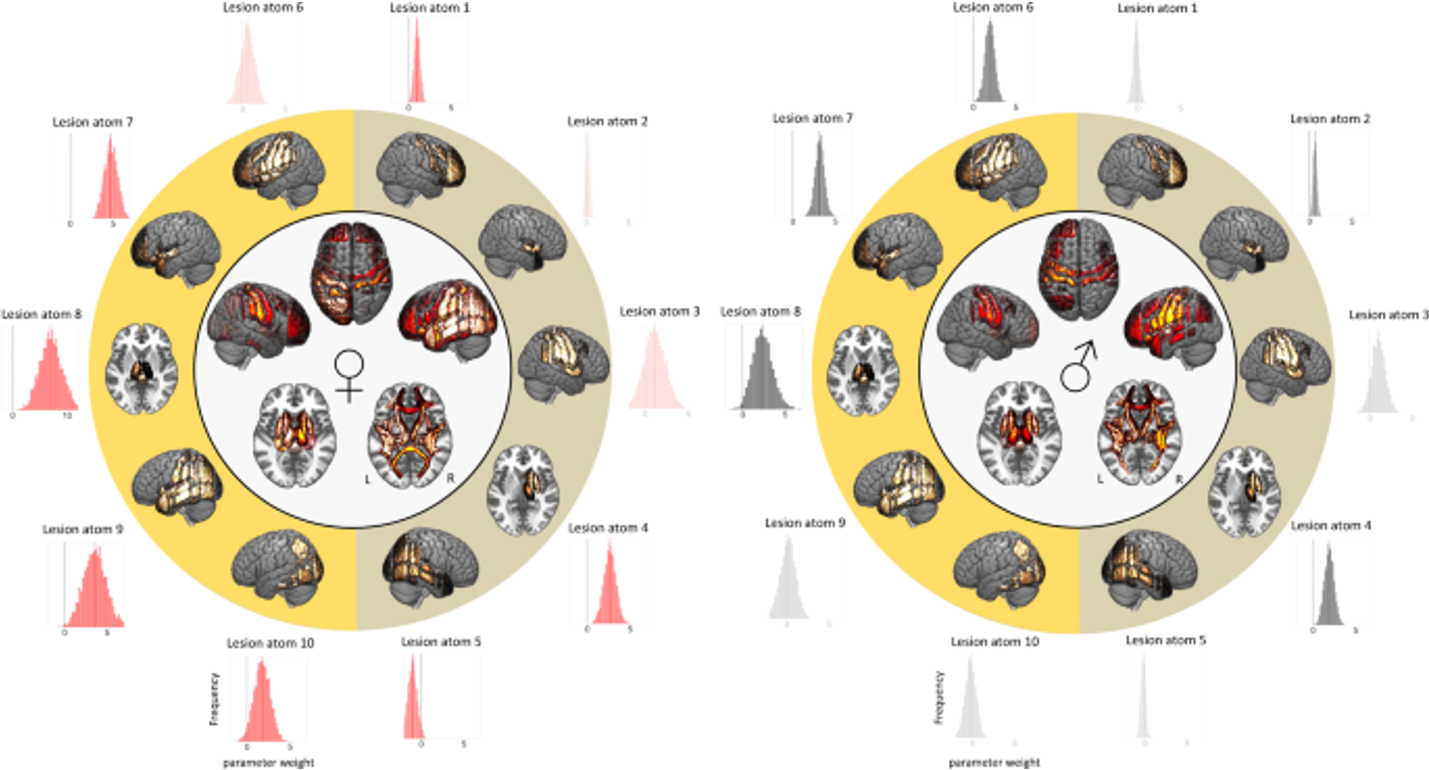
女性(左)和男性(右)中风的严重性
该研究的结果显示,在运动和语言功能区域的脑部病变有助于解释男性和女性的中风严重程度,然而更广泛的病变模式与女性患者有关。女性较高的卒中严重程度与后循环附近的左脑半球病变有关,而男性则不然。
因此,该研究结果表明,人群中存在性别特异性的大脑功能不对称,这对未来研究急性缺血性卒中的性别分层管理方法可能很重要。
原始出处:
Anna K. Bonkhoff et al. Outcome after acute ischemic stroke is linked to sex-specific lesion patterns. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
43
#缺血性#
0
#缺血性卒#
48
#卒中后#
50
学习了
71
#COMMUN#
46
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
63
写得
64