Neurology:追踪11例新冠肺炎相关意识障碍存活患者的预后:患者脑功能、结构连通性降低,但功能状况逐步改善
2021-12-07 Naomi MedSci原创
COVID-DOC后存活的患者总是能恢复意识。虽然残疾在住院后很常见,但在接下来的几个月里,功能状况有所改善。这些前瞻性的发现为COVID-Doc的预后和病理生理学提供了信息。
在2019年冠状病毒 (新冠肺炎)大流行的几个月后,这种疾病的神经系统症状被识别出来。20%的新冠肺炎患者出现意识障碍,大部分是严重感染和合并疾病的患者。严重新冠肺炎的意识障碍(COVID-DOC)可能会延长,神经恢复的预后不明朗,这种不确定性具有深远的影响——既可能对无康复机会的患者继续无意义的治疗,也可能对本有机会康复的患者停止治疗,而造成严重错误。
一些从COVID-DOC病程中恢复的病例逐渐增加,这些报告表明在COVID-DOC之后意识恢复是可能的,但他们对选择偏倚的敏感性使得恢复的可能性不确定。COVID-DOC的康复和指导预后讨论至关重要的长期功能结果均未进行评估。
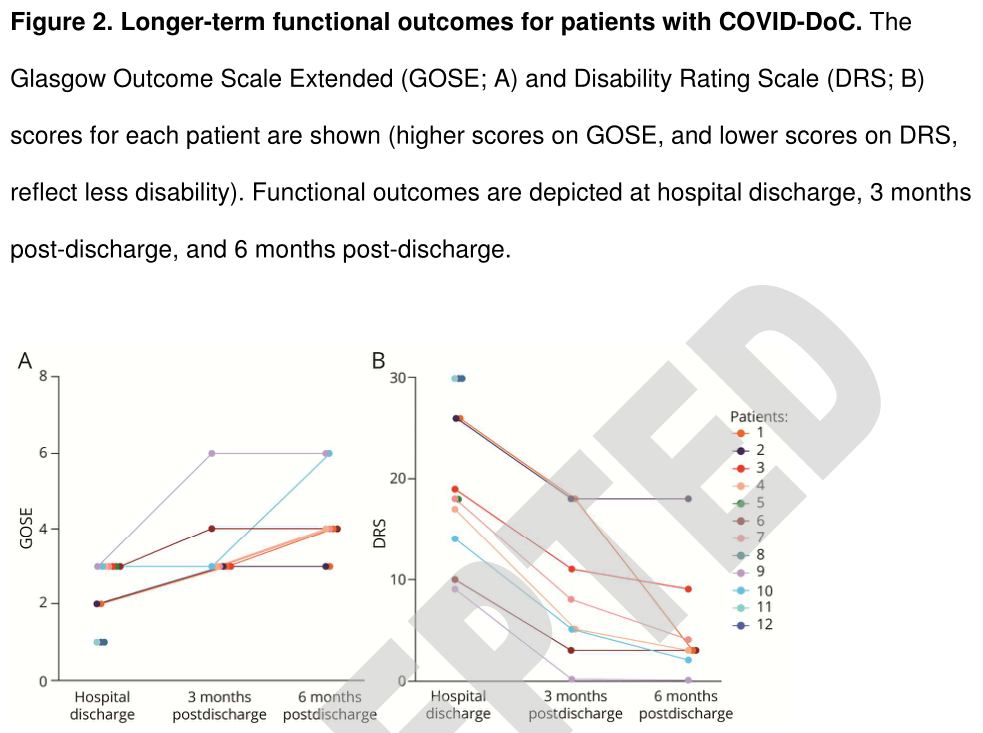
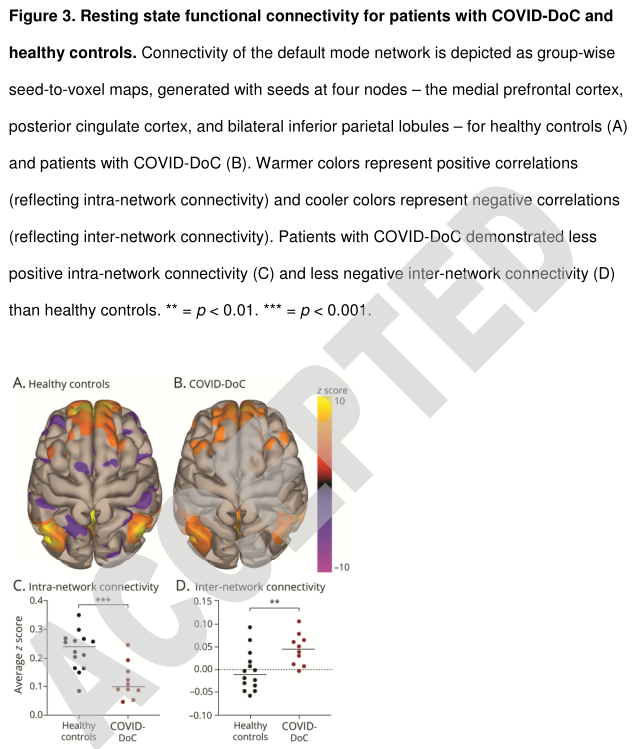
COVID-DOC的病理生理学也同样不清楚。由其他原因引起的脑损伤(无论是创伤性、缺氧性或脑血管性)引起的DOC的特征是神经连接性减弱,包括静息状态功能磁共振成像(rs-fMRI)测量的功能连接性,以及弥散磁共振(d-MRI)测量的结构连接性。尚不清楚COVID-DOC是否具有类似的连接性中断的特征。近日,有研究人员发起了一项前瞻性、纵向、多模式的研究,以描述COVID-DOC的长期康复情况,并评估其大脑连接情况(ClinicalTrials.gov NCT04476589):
(1)确定COVID-DOC患者的人口学和临床特征;(2)描述COVID-DOC术后意识和长期功能的恢复情况;(3)评估COVID-DOC与健康对照比较的功能网络连通性;(4)与健康对照对照的COVID-DOC的结构连通性评估,以及与因严重创伤性脑损伤(TBI)(已知会扰乱白质束15、16、18)的DOC患者的比较;(5)探索可能与COVID-DOC康复相关的变量。
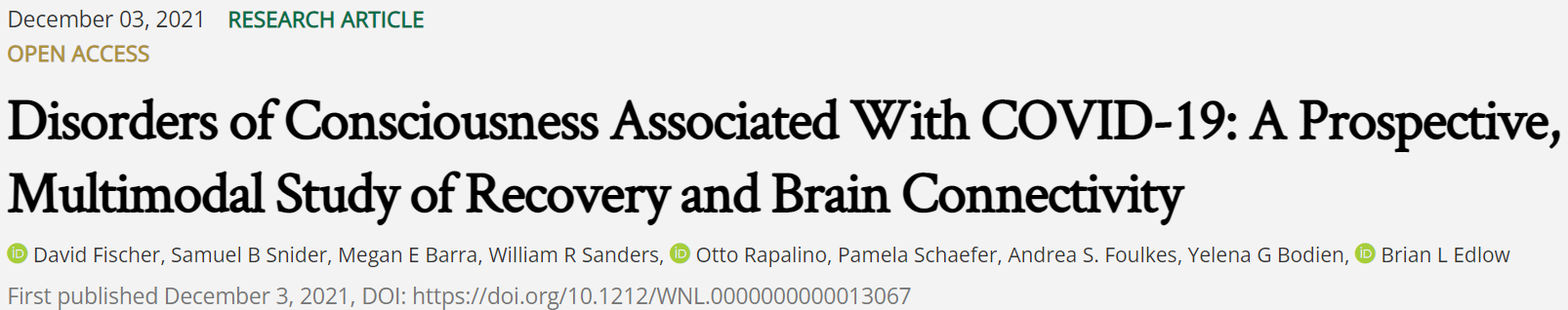
在这项前瞻性的纵向研究中,筛选了机构连续的新冠肺炎患者。招募了患有DOC的危重成人患者,这些患者因镇静或结构性脑损伤而无法解释,并计划接受脑部MRI检查。进行了静息状态功能磁共振成像和弥散磁共振成像,以评估功能和结构的连通性,并与健康对照组和严重创伤性脑损伤(TBI)引起的DOC患者进行比较。还评估了出院时及出院后3个月、6个月的意识恢复(服从命令)和功能结果(扩展的格拉斯哥结果量表[GOSE]和残疾评定量表[DRS])。还探讨了临床变量是否与COVID-DOC的康复有关。
- 在筛选了1,105名新冠肺炎患者后,共招募了12名COVID-DOC患者。中位年龄为63.5岁[四分位数范围55-76.3]。除登记后不久死亡的一名患者外,其余11名患者在停止持续静脉镇静后0-25天(中位数7[5-14.5])全部恢复意识。
- 出院时,所有存活的患者中位数Gose 3,中位数DRS 23。然而,最终除了2名患有严重多发性神经病的患者外,所有患者都带着正常的认知和轻微的残疾回到了家:3个月时,中位数Gose 3,中位数DRS7;6个月时,中位数Gose 4,中位数DRS3。
- 10名COVID-DOC患者接受了先进的神经成像;与健康对照组相比,COVID-DOC患者的脑功能和结构连通性降低,结构连通性与严重脑外伤患者相当。
COVID-DOC后存活的患者总是能恢复意识。虽然残疾在住院后很常见,但在接下来的几个月里,功能状况有所改善。虽然未来的研究是必要的,但这些前瞻性的发现为COVID-Doc的预后和病理生理学提供了信息。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Neurol#
41
学习。
52
学习学习学习学习学习学习学习学习学习学习学习学习学习
61
#脑功能#
48
#意识障碍#
61