JACC:不同主动脉病变患者心血管结局
2022-05-30 MedSci原创 MedSci原创
有动脉瘤的二叶主动脉瓣(BAV)患者更倾向与择期进行动脉瓣置换手术,相对较少需要进行动脉夹层手术。
自2007年至2016年期间,遗传性胸主动脉瘤和心血管疾病(GenTAC)注册中心招募了大量病史超过8年的由多因素引起的主动脉病变患者,以评估这类患者的心血管和手术结局。
本研究旨在比较不同主动脉病变患者因近端主动脉瘤进行择期手术及任何夹层手术的概率和年龄分布,及心血管死亡率。
GenTAC研究采用了回顾性/前瞻性设计,纳入了879位有动脉瘤的二叶主动脉瓣(BAV)患者、861位马凡综合征(MFS)患者、378位非综合征性遗传性胸主动脉疾病(nsHTAD)患者、298位Turner综合征(TS)患者、149位血管Ehlers-Danlos综合征(vEDS)患者和121位Loeys-Dietz综合征(LDS)患者。研究开始时的总体平均年龄是36.9±19.6岁。由于不同队列患者各种事件的风险不同,部分队列不到一半的患者经历同一事件(如择期近端主动脉瘤手术),因此,本研究主要比较了不同队列每个手术事件风险为25%的年龄。
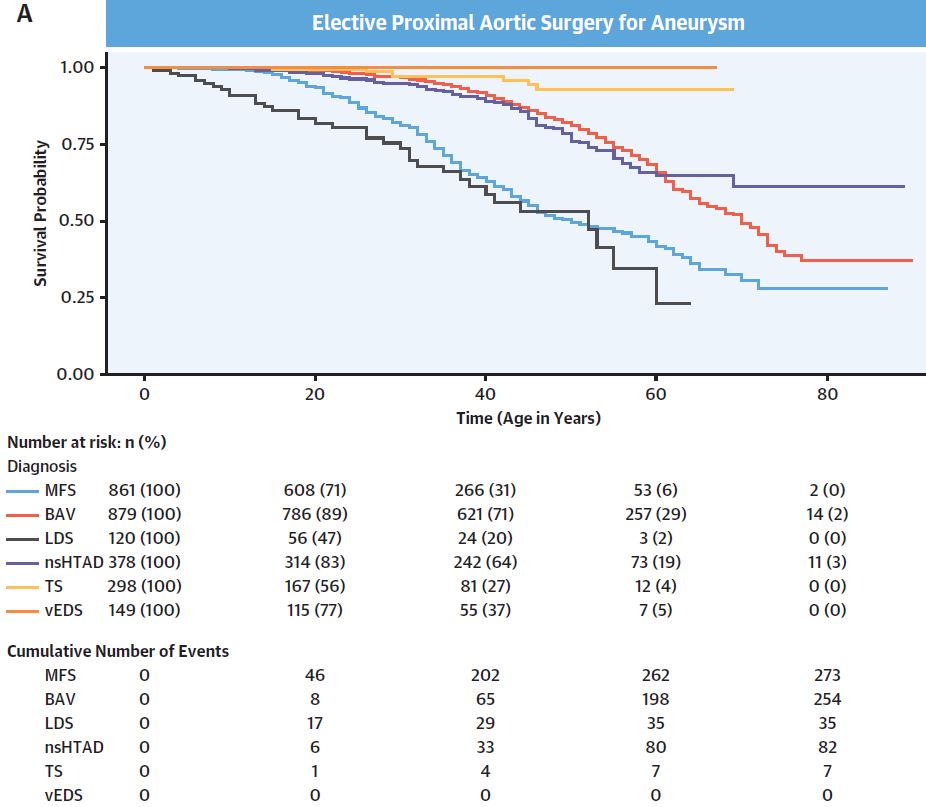
不同队列无择期近端主动脉瘤手术发生率
择期近端主动脉瘤手术在总队列中的发生率为24.2%(包括试验开始前的),其中MFS患者进行择期主动脉瓣置换术的概率最高(31.7%),其次是BAV患者(28.9%)。LDS患者有25%的概率进行择期近端主动脉瘤手术的年龄是30岁(95% CI 18-37岁),而MFS患者、nsHTAD患者和BAV患者分别是34岁(32-36岁)、52岁(48-56岁)和55岁(53-58岁)。
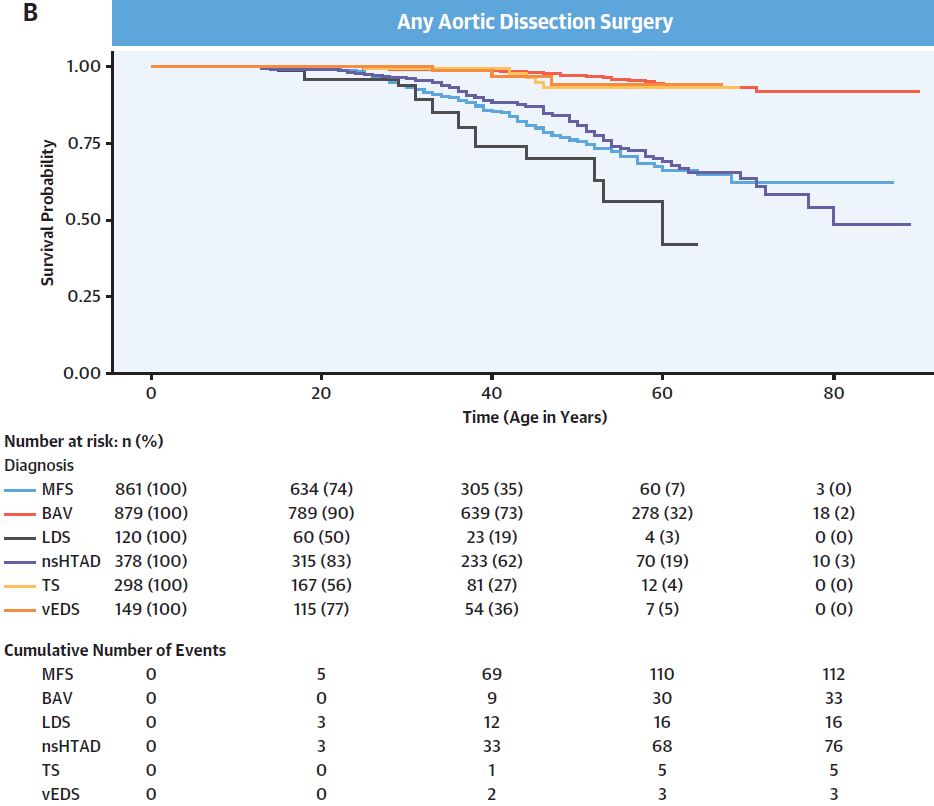
不同队列无夹层手术发生率
与MFS(13.0%)和LDS(13.2%)患者相比,nsHTAD患者队列最常进行动脉夹层手术(20.1%)。但LDS患者有25%的概率进行动脉夹层手术时的年龄最小(38岁,95% CI 33-53岁),其次是MFS(51岁,46-57岁)和nsHTAD患者(54岁,51-56岁)。
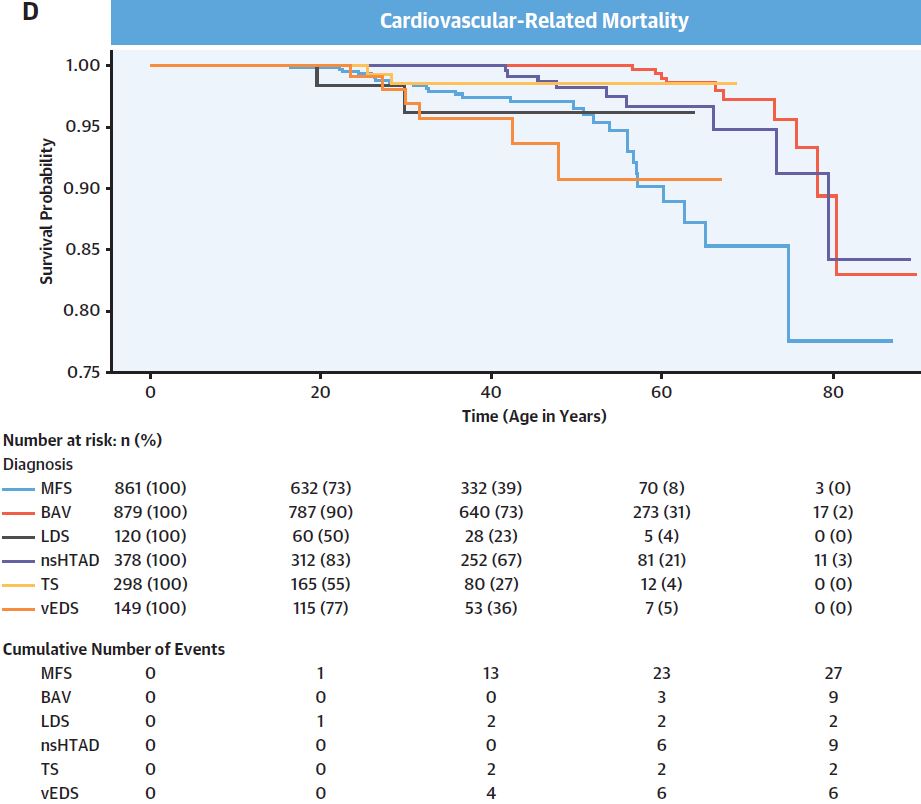
不同队列无心血管相关死亡率
BAV患者择期手术与夹层手术的比率最大(254/33=7.7),其次是MFS(273/112=2.4)、LDS(35/16=2.2)和nsHTAD患者(82/76=1.1)。与MFS患者为参考人群,BAV患者进行动脉夹层手术或心血管死亡的风险最低(HR 0.13)。最后,vEDS患者的心血管死亡风险最高(11.9/1万人·年),其次是MFS患者(9.2/1万人·年)。
综上所述,有动脉瘤的二叶主动脉瓣(BAV)患者更倾向与择期进行动脉瓣置换手术,相对较少需要进行动脉夹层手术。非综合征性遗传性胸主动脉疾病(nsHTAD)患者进行夹层手术和择期手术的概率相当,可能是因为不能早期诊断。
原始出处:
Holmes Kathryn W,Markwardt Sheila,Eagle Kim A et al. Cardiovascular Outcomes in Aortopathy: GenTAC Registry of Genetically Triggered Aortic Aneurysms and Related Conditions.[J] .J Am Coll Cardiol, 2022, 79: 2069-2081. https://doi.org/10.1016/j.jacc.2022.03.367
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#主动脉病#
0
#主动脉病变#
44
#JACC#
48
谢谢分享
36
学习了,谢谢分享
39
#心血管结局#
65
#ACC#
32
#主动脉#
47