肺动脉高压的蛋白质组学研究
2021-11-05 刘少飞 MedSci原创
肺动脉高压(PAH)是一种罕见但致命的心血管疾病,发病率和死亡率都很高。于 PAH 中蛋白质组学生物标志物和潜在分子机制及其对疾病管理价值的文献,旨在加深我们对该疾病的理解,并最终为临床应用铺平道路。
尽管治疗取得进展,肺动脉高压 (PAH) 是一种罕见但致命的心血管疾病,死亡率很高。根据新的分类,PAH 分类如下:特发性 (IPAH);可遗传(HPAH);药物和毒素诱导的;与相关因素有关,包括结缔组织病、艾滋病毒感染、门静脉高压症、先天性心脏病(CHD)和血吸虫病;对钙通道阻滞剂有长期反应者的 PAH; PAH 具有明显的静脉/毛细血管 (PVOD/PCH) 受累特征;和持续性肺动脉高压(新生儿综合征的 PH)。PAH 的发病率为每年每百万成人 2.0 至 7.6 例,其患病率从每百万成人 11 至 26 例不等。PAH 的早期临床症状是非特异性和与其他心肺疾病重叠,导致误诊或延误诊断。目前PAH的治疗策略不足,预后差,对于检测可靠的生物标志物和开发新的治疗策略无疑存在未满足的需求。
基于已知蛋白质或肽设计的蛋白质微阵列首先提高了发现蛋白质生物标志物的通量能力。然后,基于凝胶和基于 MS 的技术,包括二维凝胶电泳 (2-DE) 和二维差异凝胶电泳 (2D-DIGE),被实施为蛋白质组学的高通量技术。然而,主要的这些方法的问题是它们的重现性差、蛋白质负载能力小,并且无法检测低丰度和强疏水性的蛋白质。定量蛋白质组学可以分为鸟枪蛋白质组学和靶向蛋白质组学方法。前者可以基于质量标签进行,包括用于相对和绝对定量标签 (iTRAQ) 的等压标签、串联质量标签 (TMT) 和使用细胞培养中的氨基酸 (SILAC) 或通过计算光谱计数的稳定同位素标记,这是一种无标记定量方法。
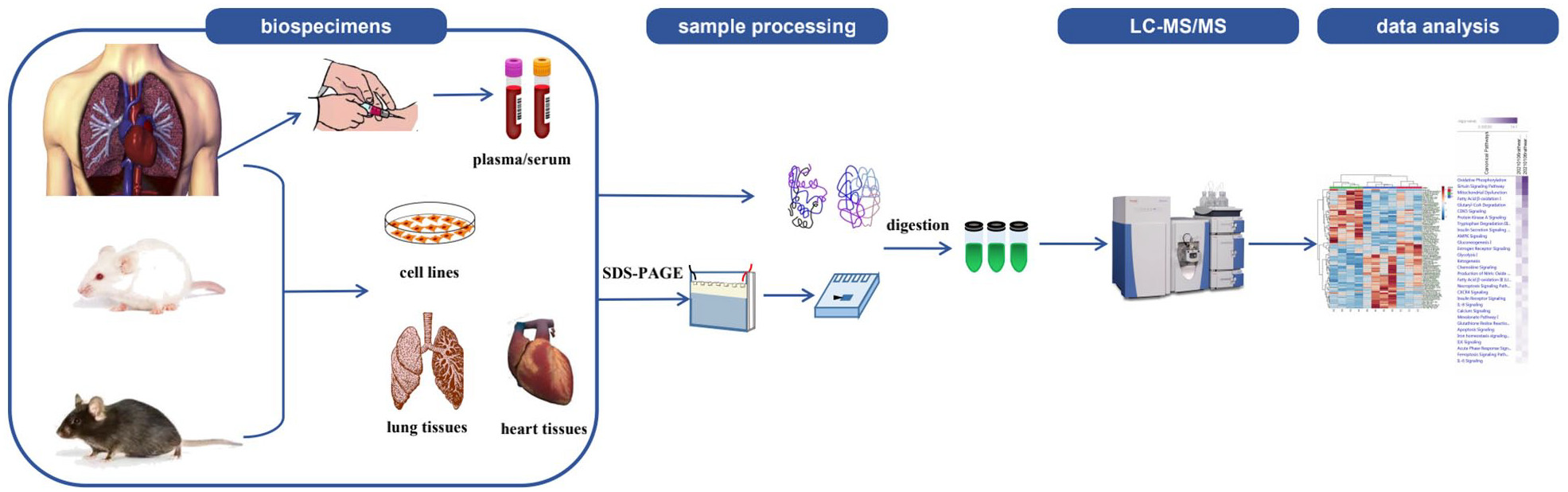
多种临床标本,包括血液(血浆/血清)、心脏/肺组织(新鲜冷冻和福尔马林固定石蜡包埋的组织块)以及来自患者或鼠模型的不同细胞类型,例如野百合碱 (MCT)-和 肺动脉结合 (PAB) 诱导的 PAH 大鼠,常用于 PAH 蛋白质组学研究。相反,迄今为止,其他体液,如尿液和支气管肺泡灌洗液,尚未用于 PAH 研究。 使用各种生物样本进行 PAH 蛋白质组学研究的经典工作流程如图下所示。
PAH 蛋白质组学分析的主要发现

蛋白质组学研究,以确定潜在临床用途的 PAH 生物标志物

蛋白质组学研究揭示 PAH 的潜在机制
PAH深层表型的蛋白质组学研究
除HPAH外,PAH亚型主要按临床特征分类,与分子生物学发病机制无关。虽然它们都属于基于 WSPH 分类的 PAH,但不同的 PAH 亚型具有共同和特定的机制。根据上述蛋白质组学研究,我们总结了 IPAH、HPAH、CHD-PAH 和 SSc-PAH 之间改变的蛋白质和途径的差异和相似之处。由国家心肺血液研究所 (NHLBI) 资助的肺血管疾病表型组学计划 (PVDOMICS, NCT02980887) 旨在使用多组学方法(基因组学、转录组学、蛋白质组学)基于分子和细胞信息对 PH 进行重新分类和深度表型分析、代谢组学、凝血组学、细胞生物组学),可以长期协助个性化诊断、预防和治疗。
总而言之,几项研究已经报道了PAH 的蛋白质组,并成功地发现了早疾病发生、诊断、预后和治疗反应中的潜在生物标志物。大多数这些生物标志物与以前接受的机制有关,但提供了更具体的分子变化的细节,如能量代谢、内皮功能、细胞生长调节、炎症和免疫系统。此外,一些新提出的生物标志物提供了对该疾病的进一步了解。尽管已经报道了许多候选蛋白质标志物和潜在机制,但很少有人深入研究并在临床中实施。从蛋白质组学研究中获得的蛋白质和机制通路是否有助于临床决策,需要在前瞻性临床队列中进行更多验证,并以基础研究为基础进行更深入的机制挖掘。多组学方法的整合对于阐明多层次的分子变化以及为进一步深入研究提供更有针对性的方向势在必行。应持续关注PVDOMICS、英国PAH队列研究联盟、美国PAH生物库联盟等大型项目的创新成果。虽然在阐明药物治疗的潜在机制和批准方面取得了进展,但蛋白质组学和翻译后修饰 (PTM) 将继续拓宽我们对 PAH 发病机制的理解,并促进蛋白质组学驱动的 PAH 精准医学 (PDPM) 的发展。最终,整合来自所有平台的数据将加深我们对该疾病的了解,并为 PAH 患者获得更好的结果铺平道路。
文章出处:
Qin X, Li T, Sun W, Guo X, Fang Q. Proteomic analysis of pulmonary arterial hypertension. Ther Adv Chronic Dis. 2021 Sep 26;12:20406223211047304. doi: 10.1177/20406223211047304. PMID: 34729151; PMCID: PMC8482352.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#白质#
37
#组学研究#
42
#蛋白质组#
50
#动脉高压#
37
#蛋白质#
42