Otol Neurotol:银屑病与听力损失和前庭功能障碍有关
2022-09-05 sunshine MedSci原创
银屑病皮损常出现在耳廓和外耳道,但中耳和内耳的表现不容易被识别。一些研究表明,听力损失和前庭功能障碍与银屑病有关,但相关程度尚不清楚。
银屑病皮损常出现在耳廓和外耳道,但中耳和内耳的表现不容易被识别。一些研究表明,听力损失和前庭功能障碍与银屑病有关,但相关程度尚不清楚。近日,发表于Otol Neurotol的一项系统回顾和荟萃分析对此进行了探究。

研究人员系统检索了PubMed、CINAHL、Scopus和Cochrane图书馆数据库,纳入的研究描述了银屑病患者的听力或前庭评估。Meta分析用几率(ORs)或平均差异(MD)表示,并设置了95%的置信区间。
结果,共纳入13项研究,涉及589名银屑病患者和617名健康对照者。银屑病患者(47.1 [12.4] 岁)和健康对照组(45.4 [11.2] 岁)之间的年龄没有明显差异。银屑病面积和严重程度指数评分为9.9(8.4),体表面积评分为7.9(14.7)。纯音测听分析结果显示,与健康对照组相比,银屑病患者所有频率的平均听力阈值较高,其中4000赫兹的差异最大(MD,7.70 [4.46-10.94];P < 0.00001)。银屑病患者的语言接收阈值更差(MD,3.53 [1.56-5.49];P < 0.0001)。银屑病患者镫骨反射异常更常见(OR,5.19 [1.68-15.99];P = 0.004)。银屑病患者的前庭测试异常在冷热试验中更常见(OR,13.12 [2.88-59.84];P < 0.0001)。对41,681名银屑病患者和80,273名健康对照组进行的另外两项研究发现,银屑病患者发生突发性感音神经性听力损失的风险更高(OR,1.50 [1.25-1.80];P < 0.0001)。
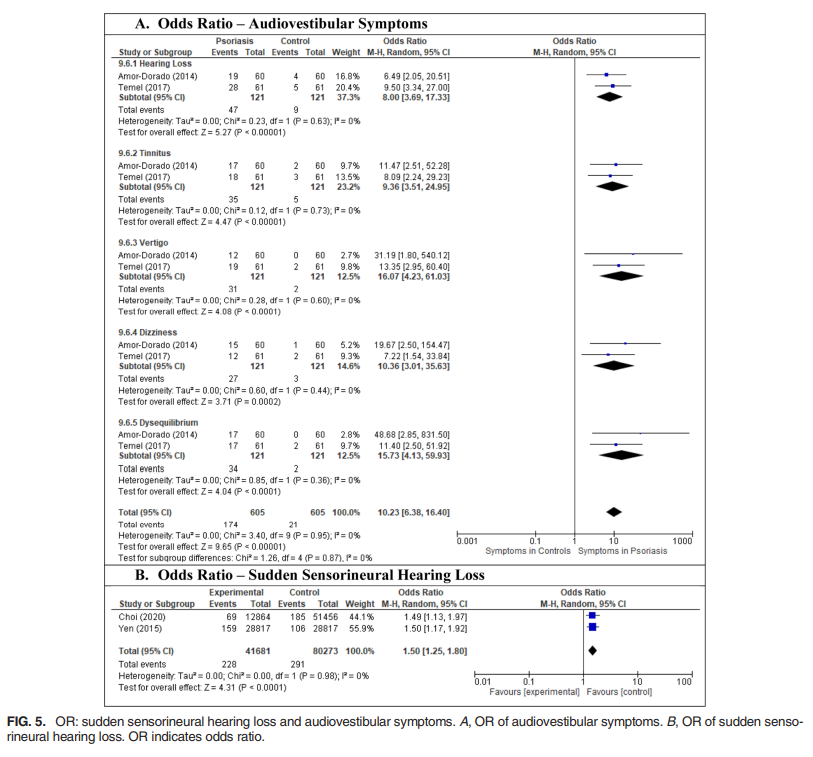
综上所述,该研究结果表明,银屑病与听力损失和前庭功能障碍有关,但临床意义仍未确定。该研究所发现的趋势需要更多的调查,病理生理学机制也需要进一步探究。
原始出处:
Seth S Jeong, et al., Otologic Manifestations of Psoriasis: A Systematic Review and Meta-Analysis. Otol Neurotol. 2022 Aug 1;43(7):742-752. doi: 10.1097/MAO.0000000000003597.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前庭功能障碍#
35
#听力#
53
#功能障碍#
50
#前庭功能#
46