Lancet Oncol:NAFLD相关肝细胞癌的临床特征及预后
2022-03-12 MedSci原创 MedSci原创
NAFLD相关肝细胞癌患者的无病生存率更高
与其他原因引起的肝细胞癌相比,非酒精性脂肪性肝病 (NAFLD) 相关肝细胞癌的临床表现和预后尚未完全明确。本研究旨在确定 NAFLD 相关肝细胞癌的患病率、临床特征、监测率、治疗分配和预后。
研究人员检索了MEDLINE和Embase数据库从开始到2022年1月17日期间收录的对比NAFLD相关肝细胞癌与其他原因引起的肝细胞癌的临床特征和预后的英文文献(横断面和纵向观察研究)以进行系统回顾和Meta分析。主要分析:i)继发于NAFLD的肝细胞癌比例;ii)NAFLD相关肝细胞癌与其他肝细胞癌的患者和肿瘤特征比较;iii)NAFLD相关与非NAFLD相关肝细胞癌的监测、治疗分配以及总体和无病生存预后的比较。
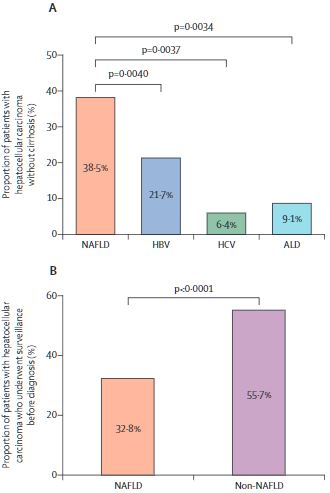
不同类型肝癌的占比
共筛查了3631份记录,其中61项研究(共包含94636位患者)符合纳入标准。总体上,继发于NAFLD的肝细胞癌病例占比15.1%。与其他原因肝细胞癌相比,NAFLD相关肝细胞癌患者的年龄更大(p<0.0001)、BMI更高(p<0.0001),也更可能会出现代谢并发症(糖尿病、高血压、高脂血症[p<0.0001])或心血管疾病(p=0.0055);NAFLD相关肝细胞癌还更可能是非肝硬化的(38.5% vs 14.6%,p<0.0001)。NAFLD相关肝细胞癌患者的肿瘤直径较大(p=0.0087),更可能是单结节性病变(p=0.0003);但Barcelona临床肝癌分期、TNM分期、甲胎蛋白水平和ECOG表现状态基本相似。
不同类型肝癌的治疗分配
与其他原因导致的肝细胞癌患者相比,NAFLD相关肝细胞癌患者的监测率较低(32.8% vs 55.7%,p<0.0001)。NAFLD相关肝细胞癌与其他原因肝细胞癌患者的治疗分配(治愈性治疗、姑息治疗和最佳支持治疗)无显著差异。最后,两组患者的总生存率没有差异(风险比[HR] 1.05, p=0.43),但NAFLD相关肝细胞癌患者的无病生存率更高(HR 0.79,p=0.044)。
综上,其他原因导致的肝细胞癌相比,NAFLD相关肝细胞癌患者无肝硬化的比例较高,监测率较低。应为有肝细胞癌高风险的无肝硬化的NAFLD患者制定适合的监测策略。
原始出处:
Darren Jun Hao Tan, et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. The Lancet Oncology. March 04, 2022. https://doi.org/10.1016/S1470-2045(22)00078-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
55
#Oncol#
56
#AFLD#
66
#Lancet#
48
#临床特征#
58
#肝细胞#
40