Front Oncol:仑伐替尼(lenvatinib)对比索拉非尼(Sorafenib)治疗晚期肝细胞癌的疗效:倾向评分匹配(PSM)分析
2021-10-26 yd2015 MedSci原创
在真实世界的临床实践中,仑伐替尼较索拉非尼降低患者的进展风险,并且安全性可控。
肝细胞癌(HCC)是世界上最常见的肝癌,也是癌症相关死亡的主要原因之一。索拉非尼(Sorafenib)是2007年批准的首个用于晚期HCC患者的药物,是一种多激酶抑制剂。索拉非尼的批准是基于两个随机、开放标签的III期临床试验,SHARP研究和AP研究,与安慰剂相比,索拉非尼显著提高了晚期HCC患者的总生存期(OS)。随机、开放标签、III期REFLECT研究显示,在不可切除的HCC患者的一线治疗中,仑伐替尼(lenvatinib)并不劣于索拉非尼[中位OS: lenvatinib为13.6个月vs.索拉非尼为12.3个月;风险比(HR): 0.92; 95%CI:0.79-1.06]。此外,与索拉非尼相比,lenvatinib尤其延长了无进展生存期(PFS)、进展时间(TTP)和客观缓解率(ORR)。根据这些来自REFLECT研究的阳性结果,lenvatinib因此成为十年来第二种批准用于晚期HCC一线全身治疗的药物。虽然lenvatinib和sorafenib均表现出良好的治疗效果,但在实际的临床实践中,对于不可切除的HCC患者应首先采用哪种药物仍是一个很大的问题。因此,来自我国台湾学者开展了回顾性研究,旨在评价真实世界中,lenvatinib和sorafenib一线治疗晚期HCC的疗效和安全性。相关结果发表在Frontiers in Oncology杂志上。

采用1:2的倾向评分匹配(PSM)分析,322例患者中(其中81例(25.2%)使用仑伐替尼, 241例(74.8%)使用索拉非尼),进一步分为仑伐替尼组(n= 70)和索拉非尼组(n=140)。PSM前,仑伐替尼组剂量减少患者比例显著低于索拉非尼组(34.7 vs 88.7%, p= 0.001)。PSM后,除了仑伐替尼的剂量减少比例(37.1 vs 90.1%, p<0.001)仍然低于索拉非尼组外,两组的基线特征是平衡的。在PSM匹配队列中,平均年龄为65.8岁,70.4%的患者为男性。在HCC的病因中,HBV感染占52.9%,HCV感染占26.7%。根据白蛋白-胆红素(albumin-bilirubin, ALBI)评分,ALBI I级患者占51.4%,II级患者占48.6%。两组患者的用药持续时间没有差异(仑伐替尼4.9个月vs索拉非尼4.5个月,p=0.779)。
PSM后,仑伐替尼组有53例(75.7%)患者肿瘤应答。其中1.9%患者达到CR, 7.5%获得PR, 52.8%发生SD, 37.7%病情进展(PD)。ORR为9.4%,DCR为62.3%。仑伐替尼组的治疗持续时间为7个月(范围:1.2 ~ 15个月)。索拉非尼组111例(79.2%)患者中,0.9%达到CR, 7.2%达到PR, 40.5%达到SD, 51.4%达到PD。
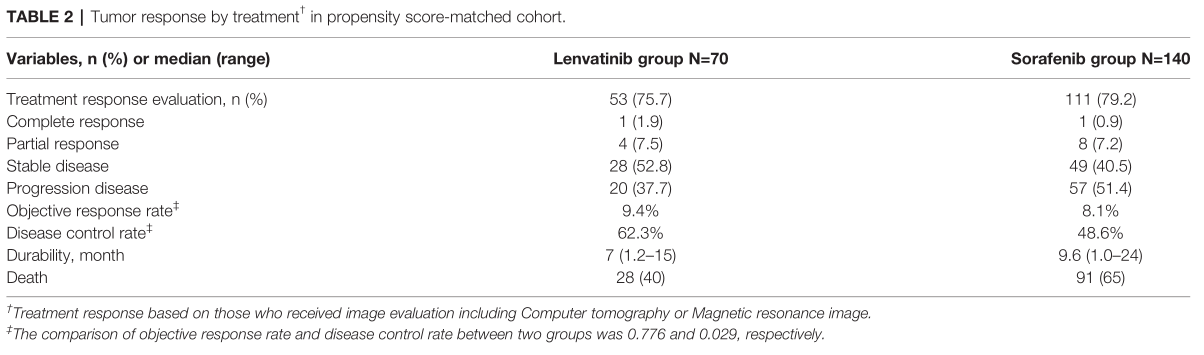
疗效评估
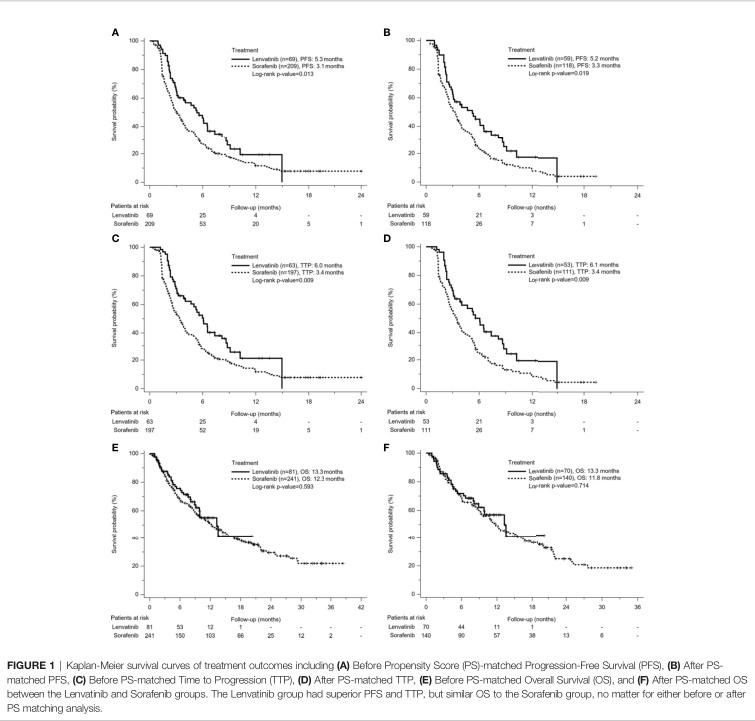
在接受放射学评估的患者中,69.6%的仑伐替尼组和88%的索拉非尼组最终观察到肿瘤进展。与索拉非尼相比,仑伐替尼治疗的患者的PFS明显更长(5.3个月vs 3.1个月,p=0.013)。在PSM匹配后,仑伐替尼的中位PFS仍明显长于索拉非尼组(5.2个月vs 3.3个月,p=0.019)。同样,无论是PSM前(6.0 vs 3.4个月,p=0.009),还是PSM后(6.1 vs 3.4个月,p=0.009), 仑伐替尼组的TTP也优于索拉非尼组。多因素分析, PSM队列中,肝功能储备差,高AFP水平,索拉非尼使用是PFS的独立危险因素。使用仑伐替尼可以减少疾病进展的风险相比 (HR=0.49,95% CI: 0.3—0.79,P<0.001)。
预后
随访期间共有181例患者死亡(56.2%),其中仑伐替尼组32例死亡(39.5%),索拉非尼组149例死亡(61.8%)。仑伐替尼组与索拉非尼组中位OS无差异(13.3 vs 12.3个月,p=0.593)。PSM匹配后,仑伐替尼组中位OS为13.3个月,索拉非尼组中位OS为11.8个月(p=0.714)。在多变量分析中,较差的肝功能储备、较高的AFP水平、疾病没有得到控制以及未接受仑伐替尼或索拉非尼治疗是PSM匹配队列中与死亡率相关的显著危险因素。无论是单因素分析还是多因素分析。
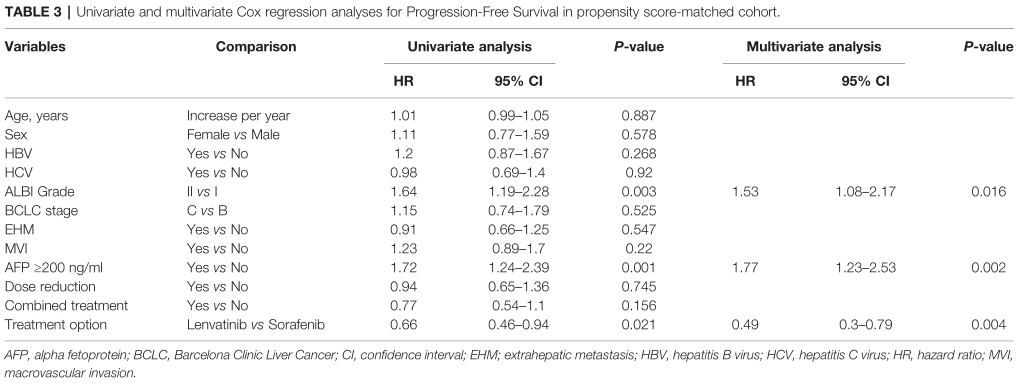
多因素PFS相关因素
PSM匹配后,亚组分析表明,所有亚组中,使用仑伐替尼的PFS优于或等于使用索拉非尼。总体而言,与索拉非尼相比,索拉非尼可降低34%的进展风险(p=0.021)。
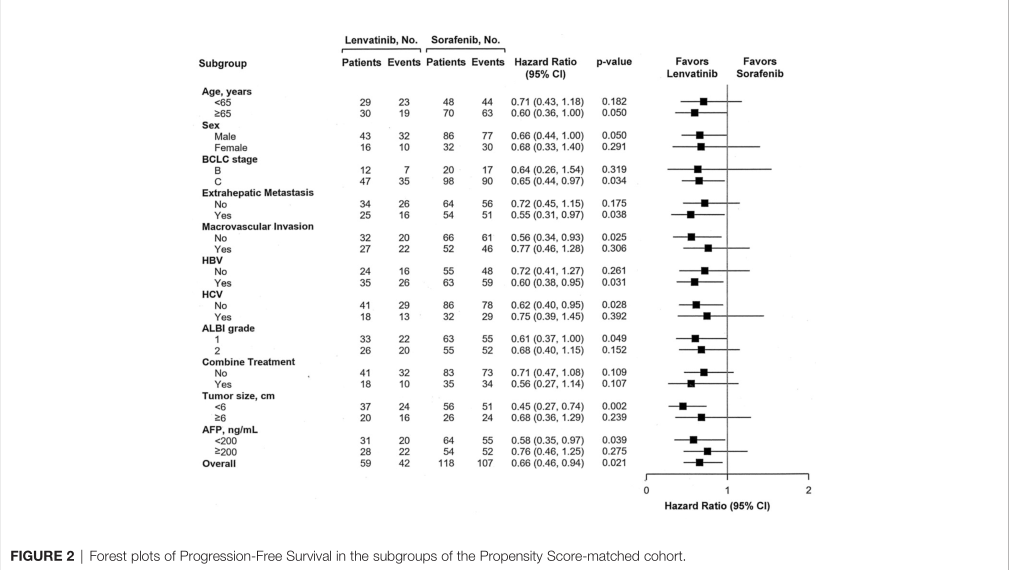
PFS亚组分析
PSM匹配后,仑伐替尼组总TRAE比例高于索拉非尼组(82 vs 75.9%, p=0.362),但差异无统计学意义。两组严重TRAE(≥3级)发生率相似(11.5vs 12%)。在仑伐替尼组中,82%的患者发生了TRAE,其中超过9%的发生率包括26.2%的患者手足皮肤反应(HFSR), 22.9%的患者高血压,19.7%的患者疲劳,9.6%的患者食欲下降。7例患者(11.5%)使用仑伐替尼出现严重TRAE≥3级者,3例HFSR。对于索拉非尼组,索拉非尼组TRAE前4位分别为HFSR(33.3%)、腹泻(25%)、疲劳(13.9%)和食欲下降(9.3%)。索拉非尼组中有13例患者(12%)出现3级TRAE,需要终止治疗;同样,HFSR是最常见的TRAE(13例中有7例)。

不良事件
综上,在真实世界的临床实践中,仑伐替尼较索拉非尼降低患者的进展风险,并且安全性可控。
原始出处:
Kuo Y-H, Lu S-N, Chen Y-Y, Kee K-M, Yen Y-H, Hung C-H, Hu T-H, Chen C-H and Wang J-H (2021) Real-World Lenvatinib Versus Sorafenib in Patients With Advanced Hepatocellular Carcinoma: A Propensity Score Matching Analysis. Front. Oncol. 11:737767. doi: 10.3389/fonc.2021.737767
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
29
#倾向评分匹配#
44
#Sorafenib#
41
#Oncol#
39
#肝细胞#
39
#晚期肝细胞癌#
42
#lenvatinib#
32