European Radiology:定量DSA在脑动静脉畸形评估中的应用
2022-08-03 shaosai MedSci原创
磁共振成像(MRI)和数字减影血管造影(DSA)是评估BAVM最常见的两种成像方式。
脑动静脉畸形(BAVMs)涉及脑动脉和静脉之间的直接沟通,可以没有症状,但通常表现为出血、癫痫发作、头痛和神经系统功能障碍。首次出现的无诱因癫痫发作有1%归因于BAVMs,而癫痫发作占BAVMs初始临床表现的20%。在最初出现癫痫发作的BAVM中,5年内无诱因癫痫复发的风险为67%。
从分布上看,癫痫性BAVMs多见于皮质位置,尤其是额颞部BAVMs患者更容易出现癫痫发作。磁共振成像(MRI)和数字减影血管造影(DSA)是评估BAVM最常见的两种成像方式。血管结构分析被用来确定BAVMs出血和发作的危险因素,其中皮质、长的引流静脉、静脉狭窄、静脉异位和浅层引流会增加癫痫发作的风险。
在血液动力学上,动脉盗血现象传统上被认为是癫痫发作的主要原因,但在多普勒研究中没有观察到这一点。相比之下,Shankar等人提出,静脉流出停滞可能在癫痫性BAVMs中起主要作用。定量DSA(QDSA)提供了一个客观且即时的血管内流动评估指标。通过使用转运时间、栓塞到达时间(BAT)或时间-密度曲线域中的瘀滞指数,QDSA有助于确定出血风险和伽玛刀放射手术的治疗反应。
近日,发表在European Radiology杂志的一项研究利用QDSA探讨了BAVMs与癫痫发作相关的血流动力学影响,并将QDSA参数与常规风险因素进行了比较,进一步阐明了BAVMs患者的血流特征与癫痫发作之间的关系,为进一步的治疗和评估提供了参考依据。
本研究从2011年到2019年纳入了104名以前没有出血或治疗的BAVMs患者,并根据癫痫发作的初始表现进行分组。每位患者的血管图和MRI结果被分析为形态特征和定量数字减影血管图(QDSA)参数。修正的脑循环时间(mCCT)被定义为同侧颈内动脉海绵段和DSA上顶静脉的栓塞到达时间之差。进行Logistic回归分析,估计BAVMs出现癫痫发作的几率(OR)。
与非癫痫组相比,癫痫组的mCCT更短(1.98秒对2.44秒,p = 0.005),更多的BAVM表现为位于颞部位置(45%对30.8%,p = 0.013)、新血管生成(55%对33%,p = 0.03)和长的引流静脉(95%对72%,p = 0.004)。在调整了年龄、性别、BAVM体积和长引流静脉后,较短的mCCT(OR:3.4,p = 0.02)、颞部位置(OR:13.4,p < 0.001)和新血管生成(OR:4.7,p = 0.013)与癫痫发作的高风险独立相关。

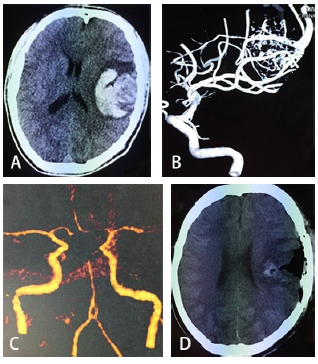
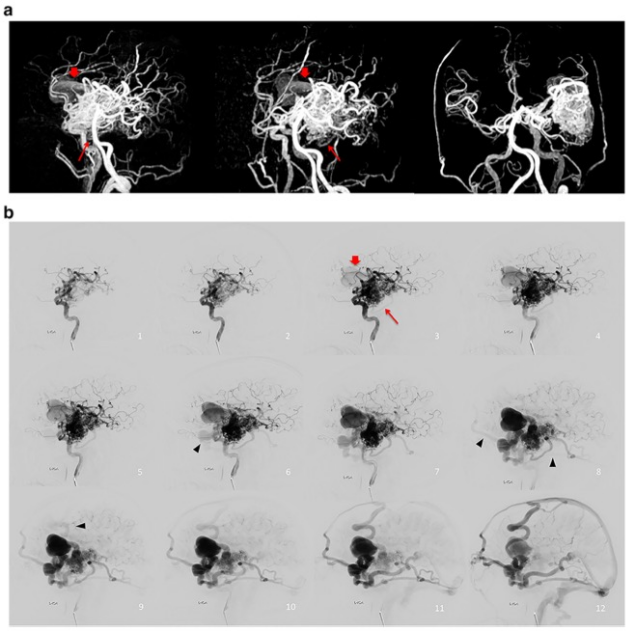
图 在出现癫痫发作(A)和没有癫痫发作(C)的脑动静脉畸形(BAVMs)患者上基于栓塞到达时间(BAT,秒)的彩色编码QDSA侧视图。两个BAVM都有长的引流静脉、动脉扩张和新血管生成。选择同侧颈内动脉(ICA)海绵窦段和顶静脉(PV)的相应时间密度曲线是(B)有癫痫发作的BAVM和(D)没有癫痫发作的BAVM。与没有发作的BAVM相比,有发作的BAVM在时间密度曲线中的修正脑循环时间(mCCT)明显缩短
本研究发现,在BAVMs患者中,较短的mCCT、颞部位置和新血管生成与较高的癫痫发作风险有关。临床上可使用QDSA对癫痫性BAVMs的脑血流动力学损伤进行客观地评估。本研究表明,血流动力学分析可以提高临床对BAVM发作的病理生理学的认识,为进一步的治疗提供了参考。
原文出处:
Jing Kai Loo,Yong-Sin Hu,Te-Ming Lin,et al.Shortened cerebral circulation time correlates with seizures in brain arteriovenous malformation: a cross-sectional quantitative digital subtraction angiography study.DOI:10.1007/s00330-022-08690-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
92
#PE#
44
#动静脉畸形#
45
#DSA#
62
#畸形#
0