子宫内膜癌保留生育治疗失败合并原发卵巢癌伴林奇综合征 1 例
2020-08-18 王益勤,戴 林,王建六 现代妇产科进展
患者,女,37 岁,因不规律阴道出血行宫腔镜下诊断性刮 宫术,术后病理示子宫内膜非典型增生。因患者要求保留生 育功能,予醋酸甲地孕酮 160mg 1 次/d 口服 9 个月,定期复 查。
1 病例简介
患者,女,37 岁,因不规律阴道出血行宫腔镜下诊断性刮 宫术,术后病理示子宫内膜非典型增生。因患者要求保留生 育功能,予醋酸甲地孕酮 160mg 1 次/d 口服 9 个月,定期复 查。后复查病理为子宫内膜复杂性增生,改 为 地 屈 孕 酮 10mg 2 次/d 和二甲双胍 0.5g 2 次/d 治疗 8 个月。再次复查 宫腔镜病理示: 子宫内膜高分化腺癌,予中药治疗半年、口服 甲地孕酮 320mg 1 次/d 治疗 3 个月,随后就诊于我院。复查 宫腔镜病理示: 子宫内膜非典型增生,局灶子宫内膜样腺癌 G1。既往体健,已婚,G0P0,否认肿瘤家族史。查体: 阴道通 畅,无异常分泌物,宫颈光滑,子宫偏大,活动可,无压痛,双 附件未触及异常包块。经阴道彩超: 子宫 7.1cm×6.3cm×5.9 cm,内膜不均回声范围 4.7cm×4.3cm×1.9cm,双卵巢( -) ,内 膜血流 RI 0.31,PI 0.37。盆腔磁共振: 子宫内膜癌 Ia 期,子 宫腺肌症可能,左侧附件囊肿。血清 CA125 42.68U/ml。入 院诊断: 子宫内膜样癌 Ia 期 G1,左附件囊肿待查。考虑患者 未生育,有强烈的保留生育意愿,前期治疗子宫内膜癌病理 无明显缓解,沟通知情后继续保守治疗,调整治疗方案,予口 服醋酸甲地孕酮 320mg,1 次/d,每 28 天皮下注射促性腺激 素释放激素激动剂( gonadotropin-releasing hormone agonist, GnRHa) 3.75mg,定期复查。治疗 3 个月宫腔镜病理: 子宫内 膜非典型增生,局灶子宫内膜样腺癌 G1。彩超及盆腔磁共 振未见卵巢囊肿。治疗 6 个月宫腔镜病理: 病变无缓解。盆 腔磁共振: 子宫下段内膜及宫颈处黏膜较前稍增厚; 左卵巢 多发囊肿,最大 1. 1cm; 子宫腺肌症可能,较前好转。血清 CA125 19.65U/ml。治疗 9 个月宫腔镜病理: 病变仍无明显 缓解; 免疫组化示: ER( 40%++) ,PR( 80%+++) ,PTEN( -) , p16( 灶状+) ,p53( 个别细胞+) ,Ki-67( 30% +) ,MLH1( +) , MSH2( -) ,MSH6( -) ,PMS2( +) 。患者进一步行外周血基因 检测示: MSH2 基因 c.518T>C( p.Leu173Pro) 杂合变异。盆腔 磁共振: 宫腔镜术后,对比前次: 子宫腔右侧部新发内膜增厚 0.8cm,考虑肿瘤复发可能大; 双侧卵巢囊肿,最大直径0.8 cm。因患者保守治疗 1 年以上疾病持续,不符合保留生育条 件,行子宫内膜癌分期手术。术中探查见: 子宫前位,形态饱 满,略增大,表面光滑,左侧卵巢可见一外生囊实性肿物直径 2cm,较糟脆,色暗红,右侧卵巢及双侧输卵管外观无异常。 留取腹腔冲洗液,先行腹腔镜下全子宫切除术+双侧附件切 除术。左附件离体后取部分送冰冻病理,并回报: 卵巢高分 化腺癌。进一步行盆腔和腹主动脉旁淋巴结切除术+阑尾切 除术+大网膜切除术。术后病理( 图 1) : 子宫内膜子宫内膜 样癌 G1,大小 1.5cm×0.3cm,侵及浅肌层,宫颈、右侧附件未 见癌侵犯; 左卵巢子宫内膜样癌 G1,左输卵管、淋巴结未见 癌侵犯,腹腔冲洗液未见肿瘤细胞。术后诊断: 子宫内膜样 癌 Ia 期 G1,左卵巢子宫内膜样癌 Ic2 期 G1,林奇综合征。术 后予紫杉醇+卡铂方案静脉化疗 4 个疗程。现术后 8 个月, 随访未见肿瘤复发。
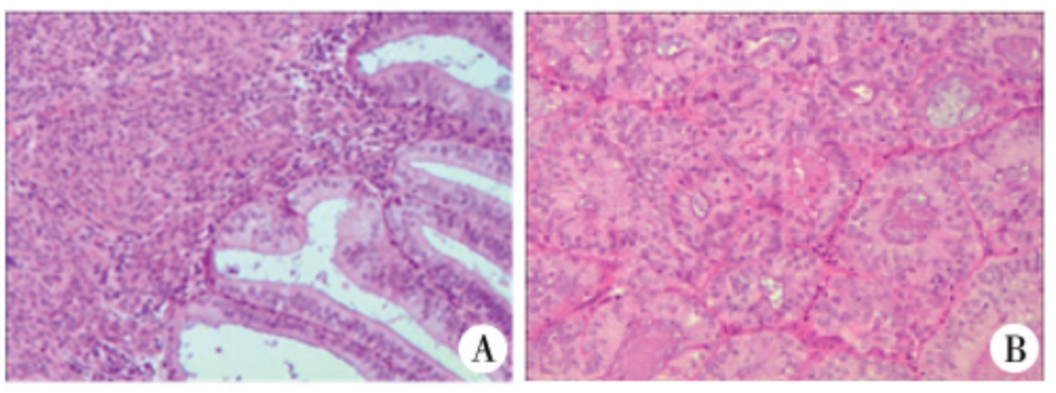
图 1 病理图片( HE×400) A: 子宫内膜子宫内膜样癌 I 级,周围子宫内膜呈分泌期表现; B: 卵巢子宫内膜样癌 I 级
2 讨 论
子宫内膜癌的标准治疗方式为全子宫和双附件切除术, 以及根据分期、高危因素酌情行前哨淋巴结切除或盆腔/腹 主动脉旁淋巴结切除术。其中 14%的子宫内膜癌患者正处 于生育年龄。对于年轻的子宫内膜癌患者,严格符合以下指 征时可考虑保留生育功能治疗: ( 1) 内膜诊刮病理为高分化; ( 2) 磁共振( 首选) 或超声提示无肌层浸润; ( 3) 影像学无可 疑转移; ( 4) 有强烈的保留生育意愿。此外,有学者建议将超 声无合并卵巢囊肿、孕激素受体高表达,作为需符合的条件 之一。 本例患者的肿瘤病理组织学为高分化,且无肌层浸润, 行口服孕激素的保留生育的治疗。治疗过程出现卵巢囊肿, 影像学未提示恶性可能,但该患者曾有 CA125 的一过性升 高,孕激素保守治疗效果不好。子宫内膜癌合并卵巢肿物时 需警惕卵巢转移或子宫内膜和卵巢同期原发双癌( synchronous primary endometrial and ovarian cancer,SEOC) 。内膜癌患者中 SEOC 的发病率约 5%,而年轻患者这一风险更高。 有作者建议,对有保留生育意愿的内膜癌患者行腹腔镜评估 附件情况,以及腹腔冲洗、淋巴结切除,以除外子宫外病变, 但行此腹腔镜手术的必要性仍有争议。韩国的一项回顾性 研究发现,年轻子宫内膜癌患者,同时性卵巢肿瘤的发生率 为 4.5%( 21 /471) ,而符合低风险标准即: 影像学评估无肌层浸 润,影像学除外卵巢恶性病变,内膜样癌 G1,CA125<40IU/ml 的 患者,无一例发生卵巢肿瘤。对于年轻低风险女性,保留生育治 疗需基于术前的严格评估,包括影像学( 磁共振、彩超) 、病理、肿 瘤标记物等,如怀疑有卵巢肿物或子宫外转移,必要时可行腹腔 镜探查。此外,应充分使患者了解保留生育功能的治疗不是标 准治疗方式,要严密监测和随访。 本例患者治疗前评估无肿瘤家族史及个人肿瘤史,但治疗 反应差,免疫组化和进一步胚系基因检测提示 MSH2 突变,但基 因突变与患者治疗反应之间是否有关,尚不明确。国际 NCCN 指南建议,拟保留生育治疗的患者在治疗前需行遗传学评估。 林奇综合征( Lynch syndrome) 是一种由错配修复( mismatch repair,MMR) 基因胚系突变引起的常染色体显性遗传病。小于 50 岁的内膜癌患者中,16% ~ 34%的年轻患者存在免疫组化 MMR 蛋白表达缺陷。因此对于所有保守治疗的年轻女性,应接受遗 传咨询,必要时行基因检测,其结果有助于评估林奇综合征相关 的其他肿瘤,以及指导亲属及后代的监测。 对于合并林奇综合征的患者能否保留生育治疗,尚无定论。 合并林奇综合征患者中内膜癌发病年龄较早,早于散发内膜癌 患者,鉴于这部分患者年轻,更倾向于保守治疗。另一方面,林 奇综合征相关的内膜癌患者,可能是由于同时存在高雌激素状 态( 如肥胖、胰岛素抵抗等) 导致内膜癌的发生,而并非基因缺陷 所致,因此这部分患者或许可从孕激素治疗获益。文献报道,2 例合并林奇综合征的内膜样癌 Ia 期 G1 年轻患者,分别予甲羟 孕酮及宫内孕激素释放系统治疗 3 个月后病理正常,1 例患者自 然妊娠,1 例行体外受精-胚胎移植,2 例均足月分娩,随后均行子 宫切除; 2 例患者均符合林奇综合征 Amsterdam II 标准和修正的 Bethesda 标准,1 例胚系基因检测为 MSH6 突变,另 1 例肿瘤组 织检测为高频微卫星不稳定( microsatellite instability,MSI) 。目 前对 MMR 表达情况与内膜癌预后相关性的结论不一。文献报 道,MMR 免疫组化异常者,更易发生晚期病变( P<0.001) ,高级 别( P<0.001) ,深肌层浸润( P<0.001) ,脉管癌栓浸润( P= 0.002) , 有更差的总生存期( P= 0.028) 和无进展生存期( P = 0.042) 。另 有文献报道,两者的复发率和生存率方面无差异。文献报道,林 奇综合征组较散发组患者的生存期更好。研究显示,MMR 蛋白 表达缺陷者的孕激素治疗反应差,其治疗缓解率低于 MMR 免疫 组化正常组( 0/6 vs 41/77,P=0.026) 。因此,目前对于合并林奇 综合征患者,能否保留生育治疗,经验尚不足。 综上所述,本例子宫内膜癌患者保留生育治疗后病理无反 应,胚系基因检测提示 MMR 缺陷,诊断林奇综合征,术后病理诊 断为子宫内膜和卵巢同时原发性双癌。保留生育多为未生育的 年轻内膜癌患者的诉求,但相较年老患者,合并卵巢同时性肿瘤 的风险增高,因此需要术前严格评估,必要时腹腔镜探查。提倡 对年轻内膜癌女性进行遗传评估,检测 MMR 蛋白或 MSI 情况, 必要时进行相关基因检测。合并林奇综合征的患者能否保留生 育,以及 MMR 缺陷对孕激素保留生育治疗疗效的影响,还需进 一步研究。
参考文献略。
原始出处:
王益勤,戴 林,王建六,沈丹华等,子宫内膜癌保留生育治疗失败合并原发卵巢癌伴林奇综合征 1 例[J],现代妇产科进展,2020,29(7)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内膜#
37
#生育治疗#
33
很有参考意义
123
#治疗失败#
45
#综合征#
32
👍
149
赞
135