J Immunother Cancer: dMMR/MSI- H胃肠道肿瘤伴有腹膜转移和腹水对免疫治疗耐药
2022-02-06 yd2015 MedSci原创
研究表明,dMMR/MSI- H胃肠道肿瘤伴有腹膜转移和腹水使用免疫检查点抑制剂(ICIs)疗效差。
近期,Journal for ImmunoTherapy of Cancer杂志上发表了一项研究结果,主要是评估在dMMR/MSI- H转移性结直肠癌(mCRC)和胃癌(mGC)接受免疫检查点抑制剂(ICIs)的患者中,腹膜受累伴或不伴腹水是否是一个不良预后因素。
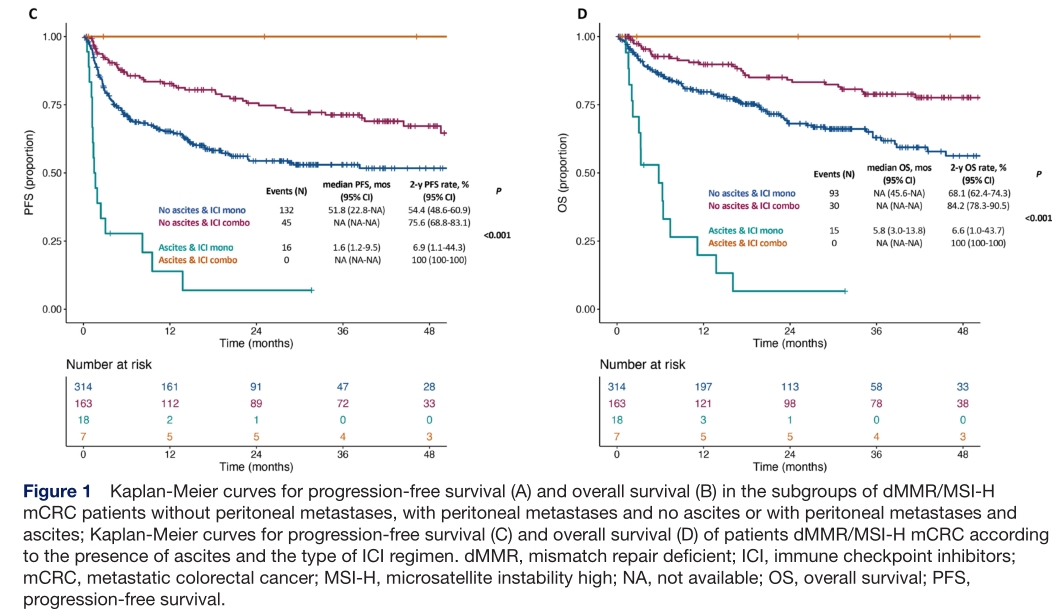
mCRC队列包括502名患者。172例(34.3%)患者存在腹膜受累,25例(5.0%)患者存在腹水。中位随访时间为31.2个月(IQR 15.6-46.0)。腹水的存在与较短的PFS和OS显著相关(两者均为p<0.001)。
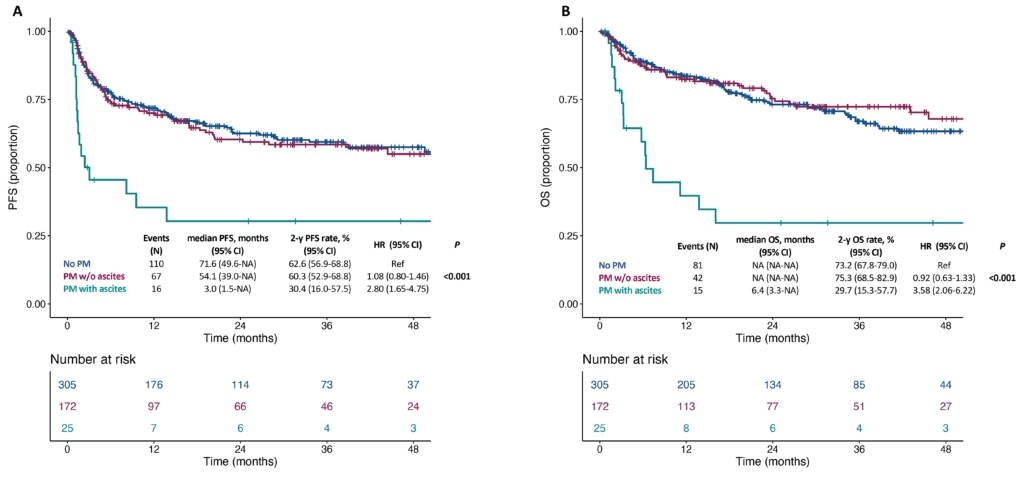
无腹腔转移的患者与伴有腹腔转移且无腹水的患者的无进展生存期(PFS)和总生存期(OS)相似(2年无进展生存期率:62.6% vs 60.3%;HR 1.08, 95% CI 0.80 ~ 1.46;2年OS率:73.2% vs 75.3%;HR 0.92, 95% CI 0.63 - 1.33),但优于伴有腹腔转移及腹水的患者(2年无进展生存期率:30.4%;HR 2.80, 95% CI 1.65 ~ 4.75;2年OS率:29.7%,HR 3.58, 95% CI 2.06 - 6.22)。
单变量和多变量分析,腹水是预后独立预后因素(adjusted HR for PFS: 2.90 (95% CI 1.70 to 4.94); for OS: 3.33 (95% CI 1.88 to 5.91))。
研究接着分析不同ICIs治疗策略(ICIs单药或联合抗CTLA-4)的影响,可见腹水患者使用ICIs单药治疗的PFS和OS最差 (中位和2年PFS率: 1.6个月和6.9%;中位和2年OS率: 5.8个月和6.6%)。无论ICIs,无腹膜转移的患者与腹膜转移且无腹水的患者的PFS和OS相似。
mGC队列包括59例患者。腹膜受累无腹水者11例(18.6%),腹水者17例(28.8%)。中位随访17.4个月后。腹水的存在与较短的PFS和OS显著相关(p<0.001和p=0.006)。无腹腔转移的患者与伴有腹腔转移且无腹水的患者的无进展生存期(PFS)和总生存期(OS)相似 (2年PFS率: 50.2% vs 61.4%; HR 1.48, 95% CI 0.55 to 4.02; 2年OS率: 56.5% vs 60.6%; HR 1.69, 95% CI 0.55 to 5.18),但优于伴有腹腔转移及腹水的患者 (2年PFS率: 17.7%; HR 4.57, 95% CI 2.07 to 10.09; 2年OS率: 26.5%, HR 4.18, 95% CI 1.70 to 10.26)。

单变量和多变量分析,腹水是预后独立预后因素(adjusted HR for PFS: 3.83 (95% CI 1.68 to 8.72); for OS: 3.44 (95% CI 1.39 to 8.53))。
综上,研究表明,dMMR/MSI- H胃肠道肿瘤伴有腹膜转移和腹水使用免疫检查点抑制剂(ICIs)疗效差。
原始出处:
Fucà G, Cohen R, Lonardi S, et al. Ascites and resistance to immune checkpoint inhibition in dMMR/MSI- H metastatic colorectal and gastric cancers. Journal for ImmunoTherapy of Cancer 2022;10:e004001. doi:10.1136/ jitc-2021-004001.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肠道肿瘤#
42
学习了
37
学习了
44
#胃肠道#
38
#胃肠道肿瘤#
57
#MMR#
45
#腹膜转移#
45
#MSI#
40
#腹膜#
42
学习
57