Nat Commun:MT1-MMP促进LDLR的剪切并加速动脉粥样硬化的发展
2021-03-28 xiaozeng MedSci原创
动脉粥样硬化这一心血管疾病是西方国家发病和死亡的主要原因之一。
动脉粥样硬化这一心血管疾病是西方国家发病和死亡的主要原因之一。既往研究显示,血浆中低密度脂蛋白胆固醇(LDL-C)的水平与动脉粥样硬化的发病风险呈正相关。LDL受体(LDLR)能够介导LDL的摄取并对于血浆中LDL-C的清楚起着重要的作用。
LDLR可以进行蛋白的水解剪切,以将其可溶性胞外结构域(sLDLR)释放到细胞外环境中。然而,负责LDLR剪切的蛋白酶目前仍然未知。
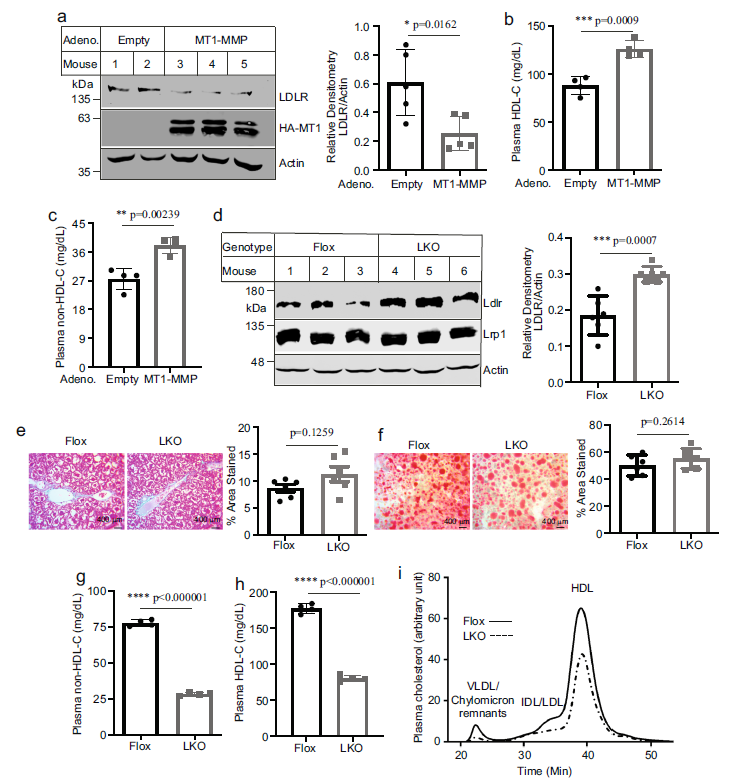
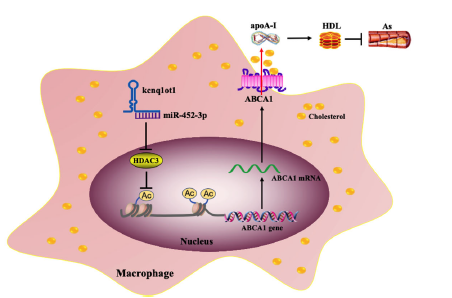
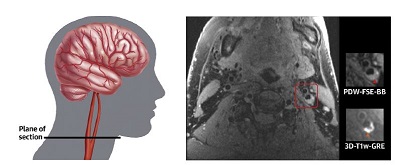
在该研究中,研究人员报告了MT1-MMP(膜类I型基质金属蛋白酶)能够与LDLR共免疫沉淀和共定位,并促进LDLR的剪切。在肝脏中缺乏MT1-MMP的小鼠模型中,血浆中sLDLR和胆固醇的水平降低,而肝LDLR的水平升高。当过表达MT1-MMP时则观察到相反的结果。
MT1-MMP调控LDLR的剪切
研究人员发现,过表达MT1-MMP显示出了动脉粥样硬化病变的增加,而敲低MT1-MMP则能够显著减少apoE(载脂蛋白E)敲除小鼠的主动脉中胆固醇酯的积累。此外,sLDLR与小鼠和人血浆中的包含apoB和apoE的脂蛋白相关。进一步的研究显示,血浆LDL-C水平高的受试者的血浆sLDLR水平显著升高。
MT1-MMP的影响
综上,该研究结果解释,MT1-MMP能够促进肝LDLR的胞外结构域的剪切,并调节血浆胆固醇水平和动脉粥样硬化的发生发展。
原始出处:
Alabi, A., Xia, XD., Gu, HM. et al. Membrane type 1 matrix metalloproteinase promotes LDL receptor shedding and accelerates the development of atherosclerosis. Nat Commun 12, 1889 (25 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
34
#COMMUN#
32
#LDLR#
31
#Nat#
37
已读,真是受益匪浅
59
#LDL#
30
好文章!
74