Lasers Med Sci:剥脱性和非剥脱性激光都可有效改善萎缩性痤疮瘢痕
2022-05-21 sunshine MedSci原创
寻常痤疮是一种慢性顽固的皮肤炎症,在青少年甚至成年人中的发病率很高。痤疮疤痕是一种常见的美容并发症,可能会给患者带来生理和心理压力,影响患者的生活质量。
寻常痤疮是一种慢性顽固的皮肤炎症,在青少年甚至成年人中的发病率很高。痤疮疤痕是一种常见的美容并发症,可能会给患者带来生理和心理压力,影响患者的生活质量。研究显示,点阵激光被广泛用于改善痤疮,根据波长的不同,FLs可分为点阵烧蚀性激光器(FALs)和点阵非烧蚀性激光器(FNALs)。近日,发表于Lasers Med Sci的一项随机对照试验比较了点阵非剥脱性1927纳米铥激光(FTL)和点阵烧蚀性2940纳米Er:YAG激光(FEL)在治疗痤疮瘢痕方面的疗效和安全性。
研究纳入患有中度或重度萎缩性面部痤疮疤痕的受试者,其左侧面部接受3次FTL治疗,右侧面部接受3次FEL治疗,平均间隔时间为4-6周。最后一次治疗后进行为期12周的随访。主要评估包括Goodman&Baron全球瘢痕定量分级系统(GBS)、自评改善和满意度评分。
结果,共有27名受试者完成了研究;FTL侧的平均GBS从基线时的11.15±5.04降至7.07±4.87,改善率为36.54%;FEL侧的平均GBS从10.81±4.46降至7.00±4.07,改善率为35.27%。不良反应包括一过性疼痛、红斑、水肿和痤疮的发生率增加。两种激光器之间没有发现明显差异。
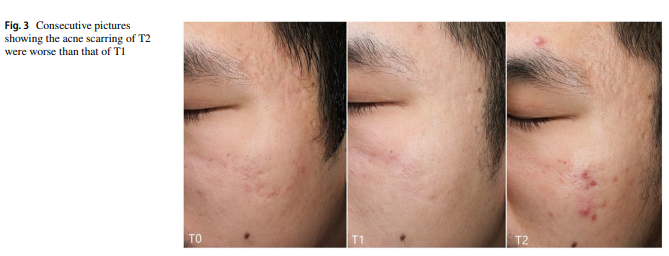
综上所述,该研究结果表明,FTL和FEL都能改善萎缩性痤疮瘢痕,而且耐受性良好。但是,激光治疗期间痤疮的发生可能对激光的疗效产生负面影响。因此,在激光治疗期间,要重视预防寻常痤疮的复发和感染。
原始出处:
Kune Lu, Suiqing Cai. Efficacy and safety comparison between 1927 nm thulium laser and 2940 nm Er:YAG laser in the treatment of facial atrophic acne scarring: a prospective, simultaneous spilt-face clinical trial. Lasers Med Sci. 2022 Apr;37(3):2025-2031. doi: 10.1007/s10103-021-03465-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#萎缩性#
39
#ERS#
43
#萎缩#
41
#激光#
44
#瘢痕#
52
#Med#
0