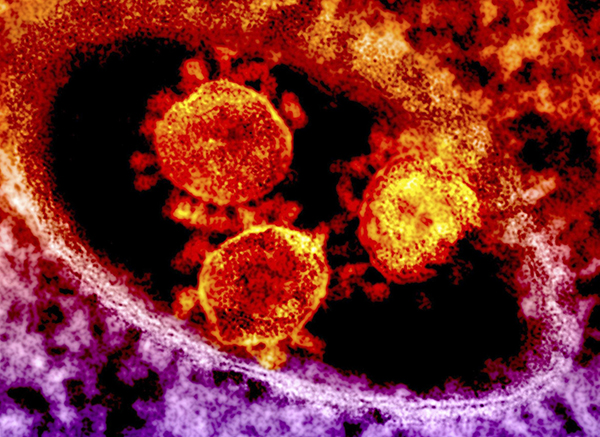
Sci Trans Med:SARS抗病毒疗法新进展
2017-06-30 佚名 Antiviral inhibits e
2017年6月29日--根据发表在最近一期的《Science Translational Medicine》杂志上的一篇文章,一类新的抗病毒药物前体具有广谱性的抑制冠状病毒(包括SARS、MERS等)的作用。这一发现为未来的相关药物开发提供了思路,或许有利于预防未来可能出现的流行病疫情。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
29
继续关注
59
#抗病毒#
24
#SARS#
31
#抗病毒疗法#
27
#Med#
16
学习了,学习了
63