JAHA:预测氢氯噻嗪血压反应性的新型标志物
2017-12-31 MedSci MedSci原创
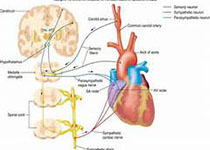
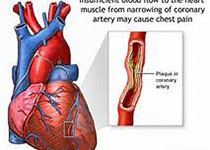
虽然氢氯噻嗪(HCTZ)是一线抗高血压药物,但是在接受HCTZ治疗的高血压患者中仅有不到一半达到了理想的血压水平,因此,寻找能预测对HCTZ起反应的生物标志物迫在眉睫。本研究的目的旨在通过代谢组学、基因组学和脂类组学的方法寻找与HCTZ血压反应相关的新的生物标志物。首先,本研究对最近研究发现与HCTZ血压反应性相关的13中代谢产物进行了pathway分析,分析结果显示鞘脂类代谢途径是与HCTZ血压
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#反应性#
38
#标志物#
30
#噻嗪#
34
#AHA#
33
#氢氯噻嗪#
32