Blood:FcγRIIA表达可加重SLE的肾炎和血小板活化
2020-08-14 MedSci原创 MedSci原创
FcγRIIA,一种免疫复合物受体,可促进狼疮性肾炎和血栓形成;FcγRIIA表达可改变SLE个体的血小板转录组并加速血小板活化。
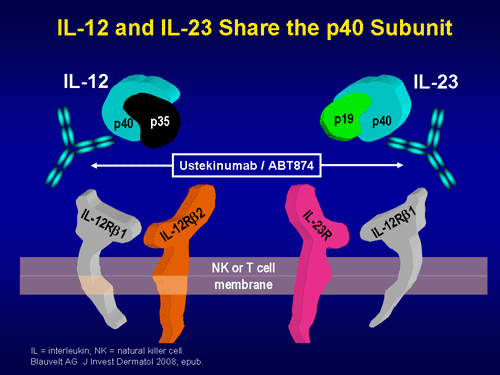
系统性红斑狼疮(SLE)是一种自身免疫性炎性疾病,特征是免疫复合物(IC)在器官和组织中沉积。在人血小板中表达的FcγRIIA,是它们对IgG抗体的独特受体,可使其对循环IC很好的应答。
虽然血小板慢性活化和血栓形成是人SLE的公认特征,但血小板活化在SLE中的确切机制尚未明确。在本研究中,Melki等研究了FcγRIIA在SLE和血小板活化中的作用。
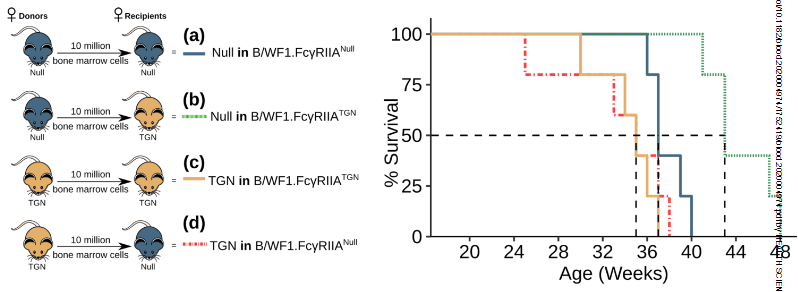
在SLE患者中,IC的水平与血小板活化相关。鉴于小鼠中无FcγRIIA存在,无论任何SLE模型小鼠的血小板对IC都无反应,研究人员将FcγRIIA(FCGR2A)转基因诱导进SLE的NZB/NZWF1小鼠模型中。
在转基因小鼠中,FcγRIIA在骨髓细胞中表达,可明显加重狼疮肾炎并加速死亡。无论是在表达FcγRIIA或不表达FcγRIIA的小鼠中,狼疮发作均可引起血小板转录组的明显改变,但在FcγRIIA表达小鼠中可观察到特异性的I型干扰素反应基因变化的富集。
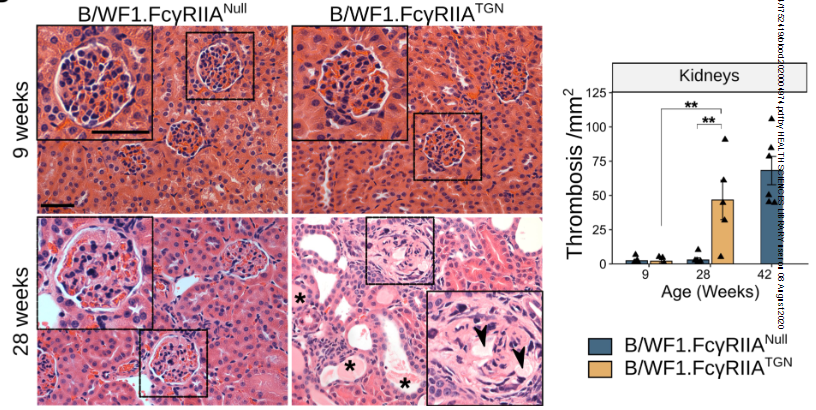
此外,在FcγRIIA表达小鼠中,还观察到了循环血小板脱粒、与中性粒细胞相互作用。FcγRIIA在狼疮小鼠中表达也可导致肺和肾脏血栓形成。
总而言之,该模型概括了人SLE的特征,可用于鉴别不同细胞谱系在SLE表现中的贡献。该研究还进一步揭示了FcγRIIA在SLE的肾炎和血小板活化中的作用。
原始出处:
Imene Melki,et al. FcγRIIA expression aggravates nephritis and increases platelet activation in systemic lupus erythematosus in mice. Blood. August 7,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好
111
优秀
97
#SLE#
25
#肾炎#
35
好
116
学习了
101