Sci Transl Med:HIV新疗法!
2018-01-26 Juka,Ruthy 转化医学网
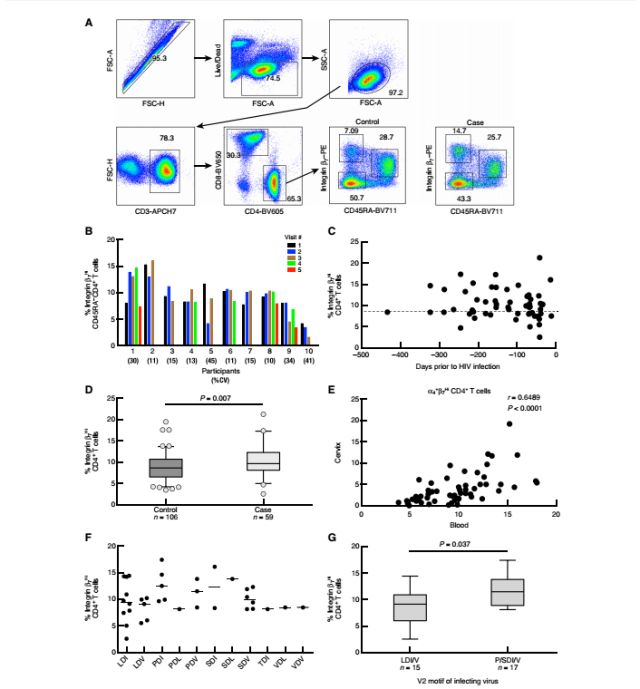
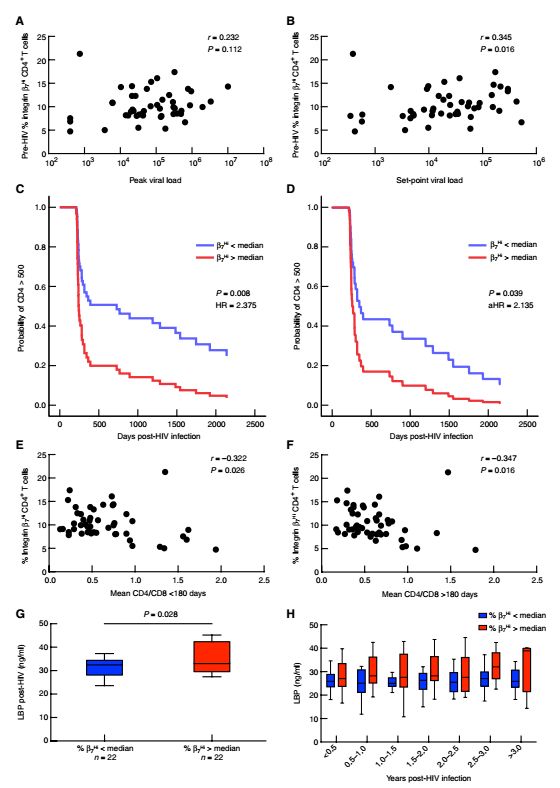
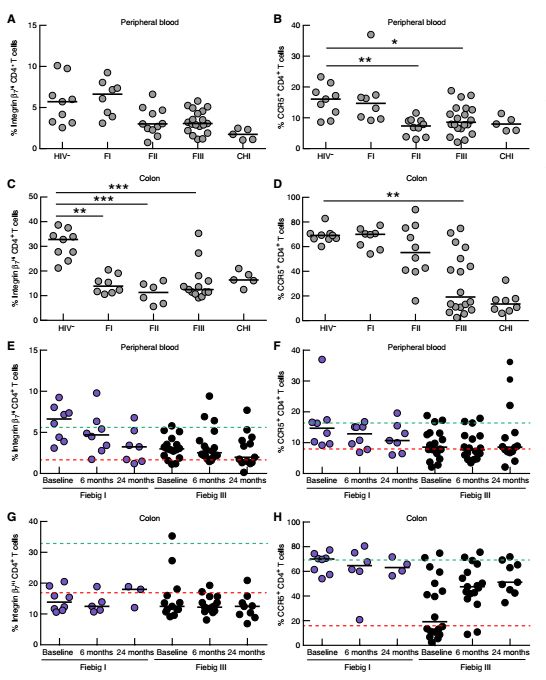
艾滋病是一种危害性极大的传染病,由HIV病毒引起。HIV是一种能攻击人体免疫系统的病毒。它把人体免疫系统中最重要的CD4+T淋巴细胞作为主要攻击目标,大量破坏该细胞,使人体丧失免疫功能,导致人体易于感染各种疾病,并可发生恶性肿瘤,病死率较高。目前常用的治疗是ART干预,但效果不佳,有研究发现,或许是肠道归巢蛋白(α-4β-7)搞的鬼。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TRA#
38
#Transl#
43
#新疗法#
35
#Med#
46
学习受益匪浅.谢谢分享
66
学习
73